MAGNESIUM & OSTEOPOROSIS
A Non- Pharmacological Approach to the Management of Osteoporosis
by Dr. Neville Wilson.
November 2014
World Osteoporosis Day is observed every year on 20th October.
The expanding incidence of osteoporosis, and its potential for serious consequences, warrants a sustained public awareness campaign that should not be limited to October, but maintained through every month of the year.
Fragility fractures in those who have diminished bone mineral density are likely to compromise healthy mobility and independence, with increased risk for morbidity and mortality.
Often the diagnosis of osteoporosis is made only after a fall has been reported and a fracture identified, or following a complaint of bone pain made by an elderly person.
While a screening DEXA scan may confirm the diagnosis, by measuring loss of bone mineral density in a vulnerable elderly subject, it may also fail to identify such mineral loss in a patient who has sustained a fracture injury, leading to a missed diagnosis of the underlying cause.

Failure to suspect, or confirm, a diagnosis of osteopenia or osteoporosis, may leave the vulnerable patient without protective nutrition or remedial intervention, exacerbating the risk for a further fracture, and increased risk of morbidity and mortality.
TREATMENT OPTIONS:
A wide range of pharmacological preparations have historically been available to Clinicians, both for the prevention and treatment of osteoporosis, and new formulations are in the pipeline awaiting FDA approval.
Available preparations include prophylactic calcium, Vitamin D, or both in combination, oestrogens, progestogens, parathyroid hormones, bisphosphonates, and the Dual Action Bone Agent, Strontium ranelate (Protelos).
Bisphosphonates, in the forms of Alendronic acid, (Fosamax) or in combinations with vitamin D3 (Fosavance), have been popular choices in the past, while newer preparations like Zoledronic acid, orally or intravenously, or subcutaneous Denosumab, and Teriparatide, are now available as therapeutic options, while combinations of these drugs are currently being tested for efficacy and safety, and FDA approval.
POTENTIAL FOR HARM:
The long term benefits of many popular drugs have recently been called into question and, with no proven mortality benefit, their continued use must be accompanied by caution, constant surveillance and careful consideration.
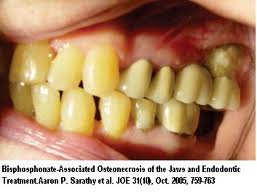
Following a systematic review by the FDA in 2012, concerns were expressed about the safety of Fosamax and Boniva, as having the potential for “rare but serious adverse events such as femur fractures, oesophageal cancer and osteonecrosis of the jaw”.
No long term benefit beyond 3 to 4 years of clinical use was demonstrated for these widely prescribed formulations.
The potential for serious adverse effects of Zoledronic acid have also been documented, and may range from mild flu-like symptoms, gastrointestinal and cardiac disturbances, to the more severe morbidities such as bone fractures, kidney failure and respiratory disorders.
A recent addition to the treatment options is Denosumab (Prolia), a monoclonal antibody, which is not without risk for major adverse events, and may cause severe renal impairment, osteonecrosis of the jaw, severe allergic reactions, or serious infections through immune suppression.
Teriparatide, also a recent addition, is a recombitant human parathyroid hormone, which appeared to improve quality of life in female subjects (EFOS), but has no long term evidence for a mortality benefit.
Its clinical effect is based on its capacity to increase the biological activity of vitamin D, in the form of 1,25(OH) 2D.
Romosozumab, following the 2014 EULAR study, was presented in Paris in June 2014, as a new formulation that stimulates bone formation and decreases bone resorption by inhibiting sclerostin activity.
This Dual Action is similar to that offered by Protelos, now discredited for its serious adverse effects, so the safety profile of Romosozumab will be under scrutiny as the clinical trial proceeds.
Another newcomer is Odanacatib, which inhibits cathepsin K, an enzyme that plays a key role in bone resorption.
Early hopes of improving bone mineral density and reducing fracture risk with Odanacatib were dashed by emerging evidence of unwanted cardiovascular effects, such as atrial fibrillation, stroke (1.4% vs 1.1% placebo) and femoral shaft fractures.
These observations must of necessity attract FDA scrutiny and put a hold on licencing approval, and possibly thwart Mercks’ hopes for the $2.5 billion profit envisaged for this novel preparation.
The search for a safe and effective remedy for osteoporosis continues, with little evidence of success, given the catastrophic consequences of drugs, once popular, now under suspicion.
NEW NUTRIENTS ON THE MARKET:
Calcichew D3 Forte Double Strength, recently launched, (0ctober 2014) represents the latest nutraceutical attempt to reduce fracture risk by addressing vitamin D and calcium deficiency in elderly adults, and provides 1000 mgs of calcium and 800 mgs of vitamin D3 (cholecalciferol).
While this, and other similar formulations, seek to address the likely deficiencies of calcium and vitamin D, in the elderly, they lack other significant and essential minerals which have experimental support for enhancing bone strength.
Not only are calcium and vitamin D required for adequate bone mineralization to occur, but magnesium and vitamin K2, are likewise, key components in the process, and a deficit of these key nutrients, is likely to impair efficient bone building, and also permit a harmful imbalance between blood and bone calcium levels, resulting in unwanted cardiovascular effects through serum calcium accumulation.
MAGNESIUM:
Magnesium is one of the 6 essential macro-minerals that comprise 99% of the body’s mineral content, and plays an essential role in energy release from food, healthy nerve function, and especially the building of strong bones.
While evidence is strong for its supportive role in healthy bone metabolism, magnesium also supports cardiovascular and respiratory functions, and has a protective role against developing diabetes, commonly associated with osteoporosis.
The role of magnesium in bone health management deserves particular attention by clinicians, with heightened awareness for low magnesium states in the elderly.
MAGNESIUM DEFICIENCY:
The World Health Organization (WHO) estimates that 75% of adults consume a diet deficient in magnesium (1) and the widespread deficiency in magnesium appears to be a significant factor in the increasing incidence of cardiovascular disease, hypertension, diabetes mellitus and other disorders. (2)
A positive correlation between magnesium and bone mineral density was shown in several studies, with magnesium deficiency resulting in decreased bone strength, diminished bone volume and poor bone development, and an excess release of calcium from bone into the blood without any new bone formation.
Magnesium deficiency is not only a risk factor for osteoporosis, but is also associated with several age related chronic disorders, such as cardiovascular disease, insulin resistance and diabetes, inflammatory disorders, chronic fatigue and even depression. (3)
Magnesium deficiency may also impair the beneficial effects of calcium supplements, raising concerns about calcium supplementation without appropriate magnesium intake.
In a 2006 study by Japanese researchers dietary calcium supplementation suppressed, rather than enhanced, bone formation in magnesium deficient rats. (4)
Reviewing the Bone Mass Density (BMD) of participants in the Framingham Heart Study cohort researchers at Tufts University concluded that an adequate dietary intake of magnesium protected against bone loss. (5)
Between one half and two thirds of total body magnesium content is stored in skeletal bone, a reservoir for several important minerals. With the passage of time this reservoir may become depleted, even though blood levels of magnesium remain constant. (3)
Magnesium deficiency may not be readily detected by clinicians examining lab reports, since as many as 50% of magnesium deficiency cases are not revealed by standard lab testing, according to the American College of Nutrition. (6)
Clinicians should not, therefore, rely on lab reports of serum magnesium, but be highly mindful of the common factors that may decrease magnesium levels in vulnerable patients, such as poor dietary intake (whole grains, leafy green vegetables, beets, legumes, dark chocolate, and a variety of herbs such as seaweed, sage, fennel, curcumin, coriander and cocoa), decreased stomach acid ( excess PPI use in elderly), Disorders of the digestive system (Crohn’s Disease, Coeliac disease), Diabetes and other Chronic disorders, and increased dietary intake of Calcium supplements.
Magnesium deficiency may also arise as a result of soil depletion caused by the widespread use of potassium fertilizers in modern agricultural methods. Potassium is a magnesium antagonist and its ubiquitous presence in farmland soil is likely to diminish the magnesium content of commonly consumed plant food.
Nutrition conscious doctors are likely to prescribe calcium-magnesium supplements in combination, when treating Osteoporosis, rather than calcium on its own, recognizing that calcium, as a pro-flammatory agent needs to be checked by its biological antagonist magnesium, acting as an anti-inflammatory agent. (7)
The absence of magnesium from popular calcium / vitamin D supplements should be a cause for concern, and may necessitate additions of magnesium, either orally or topically, for vulnerable patients.
Calcium and magnesium, in an equal or 2:1 ratio, with added colecalciferol (vitamin D3) and vitamin K2 (Menaquinone-7) are essential nutrients for maintaining bone strength, and should form part of a preventative strategy in Osteoporosis management.
A balanced diet should include 500mg of magnesium for an adult, and approximately 1000 to 1200 mg calcium daily.
MAGNESIUM AND BONE STRENGTH:
While the role of vitamin D in calcium metabolism is commonly recognized, there is scant awareness of the vital role that magnesium plays in the absorption of calcium, vitamin D, and other essential minerals, required for their conversion into active metabolites.
Magnesium enables bone and body tissue to maintain an alkaline environment, which prevents an excess of calcium loss through the urine. (8)(9) This mechanism helps skeletal bone to retain vital mineral mass and structural integrity. (10)
Magnesium also converts Vitamin D into its active form, 1,25-dihydroxyvitamin D (calcitriol) and stimulates calcitonin, which increases bone absorption and preserves bone structure, while decreasing circulating calcium which has a propensity for accumulation into soft tissues and arterial walls.
This process is dependent on the actions of magnesium and also vitamin K2, and on adequate supplies of vitamin D.
Experts in the field of bone nutrition recommend supplementing with vitamin D where sun exposure is limited or absent.
Recommendations are for supplemental doses of between 2000 IU to 5000 IU daily in order to achieve total body vitamin D status for optimal skeletal, cardiovascular, neurological and immunological health. (11), (12) (13) (14)
Magnesium has also been shown to be essential for normal function of the parathyroid gland, which controls blood levels of calcium through parathyroid hormone (PTH), and also sensitizes target tissues to PTH and active vitamin D metabolites.
Researchers have demonstrated the close relationship between magnesium and calciotropic hormones, showing a low production of active Vitamin D metabolites in magnesium deficiency. (15)
Similar disturbances in Vitamin D metabolism, as a result of magnesium deficiency, were reported by other researchers in 1988. (16)
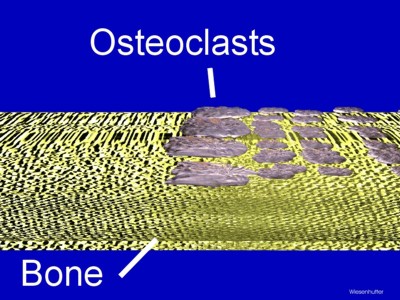
Both osteoblasts and osteoclasts, responsible for the continuous breakdown and rebuilding of bones, are dependent on magnesium for their bone remodeling function
Magnesium deficiency in animal models has been shown to result in impaired bone strength and increased skeletal fragility.
In a report from a 1999 study researchers reported that “magnesium deficiency induced uncoupling of bone formation and bone resorption resulting in a loss of bone mass” (17)
The renal enzyme, 1 alpha hydroxylase, is required to synthesize the active form of vitamin D in the kidney. Animal studies have shown magnesium deficiency to induce failure of this enzyme, resulting in decreased levels of active vitamin D.
More recently, researchers noted that a significant decrease in the number of 1,25(OH)2D3 binding sites in bone cells occurred in the presence of magnesium deficiency, explaining why patients with underactive parathyroid glands showed altered responses to vitamin D treatment. (18)
Calcium supplementation, in the absence of magnesium, may contribute to unrecognized harm through decreased absorption into bones, and also through excess accumulation in arterial walls forming calcium deposits which may accelerate atherosclerosis. (19)
CLINICAL APPLICATIONS:
Osteoporosis is a serious and potentially debilitating condition which increases the risk for morbidity and mortality in the vulnerable elderly.
Clinicians need to have heightened awareness of these risks to health, and be equally mindful of the potential for harm that is posed by some popular formulations.
Popular nutraceuticals that are devoid of magnesium and vitamin K2 should be supplemented with these essential minerals in order to secure efficacy, and to minimize their potential for adverse consequences.
Dr. Neville Wilson.
November 2014.
REFERENCES:
- WHO – Circ 1992; 86: 1475-84
- The J of Nutrition 2003 Sept; 133 (9) 2879-8
- Magnes Res 2009 Dec; 22(4):235-46
- Int J Vitamin Res 2006 May; 76(3):111-6 Matsuzaki H et al
- The Am J of Nutrition 69: 727-736, 1999, Tucker K.L.
- J of the Ac of Nutrition 2004, 23(6); 730S-731S
- The Am J of Nutrition 69; 727-736,1999, Tucker K L.
- Curr Rheumatol Rep 2007 April; 9 (1):85-92
- Am J Clin Nutr 1999 April; 69(4):727-36
- Biol Trace Elem Res 2010 Feb; 133(2):136-43
- Curr Drug Targets 2011 Jan; 12(1)4-18, Horlick M F
- Am J Clin Nutr 1999 May;69 (5): 842-56
- J Bone Miner Res Dec; 22 Supp 2:v 64-8
- Anti Cancer Res 2011 Feb;31(2):607-11
- Magnes Res 1995 Mar 8 (11);77-84
- Magnes Res 1988 Dec; 3-4:131-139
- Magnes Res 1999 Dec Dec; 12(4) 257-67
- J Phys Biochem 2004, Sept 60 (3), 1999-2003
- Lipids Health Disorders 2006, June 23, 5:6
oo000oo



Hello Dr. Wilson,
I heard about you from my daughter Caoimhe. She is a rep for Novartis. I hope you don’t mind my bothering you.
I’ve been a great believer in but D going way back. I was trying to spread the news to my educated kids who looked at me and gently quizzed my sources. Then my daughter met you, and she came home to me telling me all about you.
Now I’m on about magnesium and got k2. Thing is, how much do I take to get the balance right. I was diagnosed with osteoporosis about five years ago. I was on Fosavance until about a year ago when I read your blog. I’m taking the morepa oil as you recommended. So what magnesium and vitamin k2 is best to take? I go for a 5000 vitamin D though here in Waterford they look at me like I’m mad. Hope to visit you soon when the I’m in the area. Thanks dr.Wilson
Joan.