Dr. Neville Wilson
January 2018
YOUR THYROID GLAND:
A healthy thyroid gland is essential for overall wellbeing since it provides the necessary hormones for energy production in all living cells and tissues, including the brain.
The health and normal function of the thyroid gland is particularly important in pregnancy, since the hormones it produces are vital for the early normal development of the fetus, and for maintaining a normal pregnancy with a healthy outcome.
Since your Thyroid gland is the driver of your body’s metabolic rate, an underactive
Thyroid can slow down your normal rate of energy production, leaving you with a sense of lethargy and fatigue, often associated with difficulty in losing weight, and other debilitating symptoms, like mental dullness and poor memory, muscle aches and pains, abdominal discomfort and constipation, cold extremities, dry skin and hair loss.
An untreated underactive thyroid (hypothyroidism) during pregnancy can hinder normal fetal development and result in unexpected pregnancy loss, or a fetal abnormality.
An overactive thyroid (hyperthyroidism) by contrast, will cause an increase in metabolic rate, often associated with a rapid heart rate and palpitations, and be followed by a visible tremor and weight loss. In severe cases a “thyroid storm” may occur requiring emergency treatment.

A thyroid gland that is underactive, (hypothyroid) or overactive (hyperthyroid), may lead to a host of unpleasant and unwelcome symptoms, affecting any one of a number of organ systems, which may be either mild, or severe in some cases, resulting in such disability that normal daily activities become almost impossible.
Thyroid hormones are synthesized by the thyroid gland and are critical regulating molecules with important roles in human physiology and development, including fetal and post natal nervous system development, as well as the maintenance of adult brain function.
The effective management of hypothyroidism and hyperthyroidism may not always be easy, and may present a challenging task for the doctor, often necessitating personal involvement by the patient, with a degree of responsibility for self care in terms of diet and lifestyle habit, in order to create the favourable circumstances for maintaining a healthy thyroid, or healing and restoration, with reversal of symptoms in the case of thyroid disorder.
Both overactive and underactive thyroid glands may be the result of circulating thyroid antibodies, causing either Graves Disease (Hyperthyroidism) or Hashimoto’s Disease (Hypothyroidism).
Overt hypothyroidism may result in a host of pregnancy related losses. (4)
Hypothyroidism may be caused by any one of the following conditions:
(a) Autoimmune Thyroiditis (Hashimoto’s)
(b) Radiotherapy or surgery.
(c) Congenital defect.
(d) Drugs, Lithium or Amioderone.
(e) Iodine deficiency
(f) Infiltration diseases.
(g) Pituitary or Hypothalamus diseases.
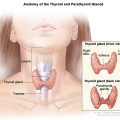
The Thyroid Hormones T3 and T4 :
The two major hormones produced by the thyroid are T3 (3,5,3’-triiodo-L-thyronine) and T4 (3,5,3’,5’-tetraiodo-L-thyronine (thyroxine), and these hormones mediate central nervous system (CNS) effects, primarily through thyroid hormone receptors (TRs), which then bind to genes that regulate the actions of certain proteins, known as co-regulators.
The thyroid gland also produces calcitonin, a hormone that helps to maintain normal levels of serum calcium and phosphorus.
T4 differs from T3 by having an additional iodine atom at the 5’ position of the thyroxine ring, and appears to function as a pro-hormone prior to its conversion to T3, the more biologically active form.
It is not known whether T4 can also function as an active hormone in the brain. T4 has, however, has been shown to cross the blood brain barrier (BBB), and there is evidence for both T4 and T3 activating TRs in the brain.
It is the removal of this 5’iodine atom from T4, by the deiodinase enzyme system, which creates biologically active T3, and enables the further synthesis of T2 and T1 to take place in the peripheral cells. (1) (2)
The traditional treatment by medical doctors, of an underactive thyroid (hypothyroidism), is replacement hormone therapy with a synthetic form of Thyroxine (T4), by prescription drug Eltroxin, which is effective in most cases, serving to support thyroid function in the peripheral cells.
Thyroxine is primarily T4 (97%) and T3 (3%), and needs further conversion to provide a sufficient supply of the biologically active T3 to the peripheral cells.
Some people, however, have a defective deiodinase gene which prevents the necessary conversion of T4 to T3, rendering them deficient in active thyroid hormone, and dependent on T3 supplementation, without which they will experience all the unpleasant symptoms of thyroid hormone deficiency.
In these cases, whether pregnant or non pregnant, standard medication with T4 (Thyroxine) does not satisfy the body’s requirements for T3, causing persistence or worsening of their symptoms, until they are given either T3 supplementation, or combined T4/T3 supplementation. (Naturethroid, NP Throid, Westhroid)
The failure to restore a sense of well being in patients with an underactive thyroid by medicating only with T4 (Thyroxine), can be a source of concern and confusion, for patients and doctors alike, since reliance on standard thyroid lab results on which standard therapy is based, do not always reveal the true nature of thyroid hormone activity in the peripheral cells, and may continue to appear within the reference range and judged as being “normal”.
Other causes for failure to convert T4 to T3 will be discussed later in this article.
(2) Thyroid Hormone Reference Ranges :
The traditional assessment of thyroid function is based on lab results which generally report TSH levels, and may in some cases include a T4 level.

Very rarely is a T3 level reported, unless specifically requested by a medical doctor who is familiar with thyroid disorders, and the Lab’s willingness to process this request.
Many patients in Ireland report an unwillingness by their primary care doctors to obtain T3 levels, or to repeat Thyroid antibody levels, not realizing that antibodies can undergo changes.
Many patients who have done their own research will demand a T3 level in addition to TSH and T4.
In many reported cases only the TSH level is supplied, and if within a “normal reference range” is invariably interpreted by the consulting doctor as being “normal”, and the patient subsequently informed that replacement therapy “is not required”.
In a large number of reported cases patients have been offered prescriptions for anti-depressant drugs, following suggestions by their doctor that they are suffering from depression, and not a thyroid disorder. These patients object to this analysis, insisting that they are not chemically depressed. (See my article : Your Thyroid and Depression).
It is not uncommon for patients, in these cases, to request further testing from more specialized labs, and to seek medical support form practitioners who are familiar with thyroid problems.
Current reference ranges, as used by most labs, reflect average blood levels within the general population, but may fail to take account of the impact of a toxic environment, or other factors, on populations regarded as “normal”.
Research in the UK and USA shows that the individual normal range of thyroid hormones is not always the same as the population reference range, (3) a fact that must be accounted for in the management of thyroid disorders.
An average lab may report the following reference range as being the norm, and by which thyroid function is judged to be either underactive (hypothyroid) or overactive (hyperthyroid), and on which basis medical treatment is generally prescribed.
TSH : 0.5 – 5.0 mIU/L
T4 : 12-22 pmol/L
T3 : 0.1-6.8 pmol/L
While most labs in Ireland and the UK report TSH levels within the above reference range (0.5-5.0 mIU/L, (or even higher in some labs) as being normal, there have been concerns that this range is too wide, and should be reduced to a narrower range in order to identify patients at risk of being hypothyroid.
Some international labs have modified the reference range for TSH to be 0.3-3.0 mIU/L. (See my article “Hypothyroidism-Detection, Diagnosis & Treatment at www.drnevillewilson.com)
It is a common mistake to assume that thyroid dysfunction is solely a thyroid gland problem that can be “fixed” by drugs, instead of correctly discerning it to be a multi-system disorder than can only be corrected by a multi-system approach, which may require drastic lifestyle and dietary changes, and the inclusion of supportive nutrients that have been shown to support thyroid function.
In some cases patients with a clinically underactive thyroid appear to manage their disorder through careful attention to lifestyle, stress relief, dietary and nutritional support, rather than by succumbing to prescribed forms of medication without attention being given to underlying factors which may impact on normal thyroid function.
(3) The Thyroid and Pregnancy:
Since pregnancy involves two persons, the wellbeing of mother and fetus must be established before, throughout, and after the conclusion of the pregnancy.
Maternal and fetal well being will require adequate and appropriate nutritional support, prior to and throughout the pregnancy, as well as an environment that is emotionally and physically secure, and free from external threats, such as environmental toxins and harmful food choices, that can adversely impact on the normal metabolic functions of every organ, and ultimately affect thyroid gland function.
Pregnancy has a significant impact on the hypothalamus- pituitary-thyroid (HPT) axis, and may be associated with marked changes in the demands for serum thyroid hormone concentrations.
With increasing human chorionic gonadotrophin (hCG) concentrations in the circulation during pregnancy, serum hormones thyroxine (T4) and triiodothyronine (T3) levels, which are bound to proteins, are increased during the first half of the pregnancy, and may be maintained to the end of the pregnancy (parturition).
Free Thyroid hormone levels (FT4 and FT3), which are unbound to protein, may decline, causing a compensatory increase in thyroid stimulating hormone (TSH), which may signal a hypothyroid state, requiring supplemental hormone therapy.
(4) Thyroid Hormones and Pregnancy:
Women who have been previously diagnosed as having an underactive thyroid (hypothyroidism) need to be carefully assessed before and during their pregnancy, as well as during the postnatal period, for changes in their TSH, (Thyroid Stimulating Hormone) in order to assess that thyroid hormones, T3 and T4, are being adequately delivered to the developing fetus and placenta.
The fetal brain requires an adequate supply of thyroid hormones for normal development, and failure to meet this physiological need may result in pregnancy loss.
Thyroxine (T4) is often described as a “pro-hormone”, since it needs to be converted into the biologically active form of T3, a process which takes place in peripheral cells of several organs.
During pregnancy there is a 30%-40% increased demand for thyroid hormone intake, because of the increased placental uptake and increased maternal blood volume and proteins, necessitating an increase in maternal thyroid hormone replacement.
The maternal production and supply of thyroid hormones (T3 and T4) will necessarily increase during the first trimester, often resulting in a sight increase of 10% to 20% in the size of the maternal thyroid, which is not necessarily problematic, unless the supply is inadequate due to an underactive thyroid, in which case the thyroid gland may be further enlarged by as much as 40 %, and present as a noticeable swelling in the neck.
Thyroid gland enlargement is due to an increase in thyroid binding globulin (TBG) and albumin due to increased synthesis in the liver.
TBG reversibly binds T3 and T4 and carries them in the bloodstream to peripheral cells where they are released in the form of Free T3 and Free T4, being in the unbound form.
The protein bound T3 and T4 are measured as total T3 and Total T4.
This enlargement of the maternal thyroid gland , accompanied by changes in the maternal blood hormone level, will reflect the need for additional maternal thyroid hormone replacement, and careful monitoring throughout the pregnancy will be required to prevent the threat of pregnancy loss, with appropriate increases in hormone supplementation made as determined by blood levels of TSH, T3, T4.
Low or insufficient levels of these hormones create a state of hypothyroidism, while an excess results in a state of hyperthyroidism.
Both hypothyroidism and hyperthyroidism are associated with increased risk of pregnancy loss, with a 2-fold increased risk in cases of autoimmune thyroiditis (Hashimoto’s Thyroiditis). (4)
Pregnancy loss may be a miscarriage, or recurrent miscarriages, or fetal death in utero during the first or early second trimester.
The prevalence of subclinical and undiagnosed overt hypothyroidism with recurrent miscarriage, late miscarriage and still birth was assessed in 262 females attending the Pregnancy Loss Clinic in Ireland in 2013.
The average age of the females was 35 years, and subclinical and undiagnosed overt hypothyroidism was found in 11.5%, while 22 women (8.39%) had subclinical hypothyroidism, and 8 women (3.05%) had undiagnosed overt hypothyroidism. (5)
In my own clinic I have recorded a large number of pregnancy losses associated with undiagnosed and untreated hypothyroidism in pregnancy.
(5) The First Prenatal Visit:
Thyroid hormone levels in the pregnant state differ from those in the non – pregnant state, and need to be carefully assessed before, throughout and at the conclusion of the pregnancy in order to support a healthy outcome.
All first visit prenatal assessments must include a Full Blood Count (FBC) with assessment of maternal serum iron and total iron binding capacity (TIBC), as well as ferritin and haemoglobin levels, since adequate iron stores are a prerequisite for efficient conversion of T4 into the more biologically active hormone T3. (More about this later)
A maternal history should also record any previous pregnancy difficulties or problems, such as infertility, miscarriages or pregnancy loss through miscarriage or fetal death.
Patients with a history of hypothyroidism should have a full thyroid panel assessment which includes tests for thyroid antibodies,(TPO and TgAB) as well as the standard TSH, T3 and T4 levels, and a reverse T3 (RT3) where possible. (only specialized labs will offer this service).
Thyroids antibodies TPO attack the thyroid cells, causing damage which may give rise to low levels of hormone secretion and hypothyroidism (Hashimoto’s Thyroiditis).
Vitamin D3 levels, Vitamin B12 and serum folate (not folic acid) levels also need to be evaluated. Serum folate and Vitamin B12 should be in the methylated form to ensure bio-availability.
Patients with hyperthyroidism (Graves Disease) should have Graves antibodies (TSI and TRAB) evaluated.
We routinely include Vitamin D3 (25OHD2), Vitamin B12 and serum Folate assessments in our clinic because of their supportive role in the supply of essential nutrients during pregnancy, and also for the conversion of T4 to T3 in the maternal circulation.
A low level of Vitamin D3 is considered to be a predisposing factor in autoimmune thyroid disease, and was shown to be reduced in patients with thyroid autoimmunity. (6)
The importance of DHA omega-3 supply for healthy development of the fetal brain is also emphasized at this stage..
TSH monitoring throughout pregnancy is mandatory.
Contrary to some common perceptions, TSH is not a thyroid hormone, but a pituitary (brain) hormone, and is produced by the Pituitary Gland in response to secretions of TBG from the hypothalamus, which in turn prompts the thyroid gland to secrete T3 and T4 on demand.
The Hypothalamus – Pituitary – Thyroid connection represents the HPT axis, which is responsible for feedback mechanisms, so that when thyroid hormones fall, TSH increases, and when thyroid hormones are elevated, TSH is suppressed.
TSH is therefore a guide as to how well the thyroid gland is functioning, and a low level will usually indicate an adequate production of T4 from the thyroid gland, while a high level may indicate an underactive thyroid gland requiring supportive thyroid hormone treatment.
In the non-pregnant state TSH is frequently used as an indicator of thyroid status by many doctors, followed by assurances to their patients that a TSH within “normal range” is indicative of no need for medical intervention or hormone replacement therapy.
This is an inaccurate interpretation of TSH, since TSH does not reveal the true status of thyroid secretion, and may be “within normal range” even in cases of severe undetected hypothyroidism, and associated symptoms, as will be explained later.
In the pregnant state TSH becomes a significant indicator of the increased demands for thyroid hormones, and should be lower than what is regarded as “normal” in the non – pregnant state.
(6) The Role of TSH in Pregnancy :
As stated above, TSH is not a thyroid hormone, and sole reliance on its blood level may mask important fluctuations in thyroid hormones T4 and T3, as well as downstream thyroid hormones, T2, T1 and RT3 (Reverse T3).
An added problem is that reference ranges for “normal” TSH levels vary from lab to lab, with no universal agreement about what a safe normal range is.
In the pregnant state TSH does provide a good indicator of adequate thyroid hormone supply, and should be kept in the lower range, (compared to levels in the non-pregnant state) under 2.5 mIU/L, to ensure that the increasing demand of T4 and T3 are being met by the advancing pregnancy.
A higher TSH, greater than 2.5 mIU/L, may represent low or inadequate levels of hormone production by the thyroid gland, with greater risk for pregnancy loss.
Many labs worldwide, consider a TSH level between 0.45 and 4.5 mIU/L as normal, and some labs have been noted to widen this range from 0.45 to 5 mIU/L. leading doctors to ignore TSH levels until they are either 5 mIU/L or even higher .
Studies show that this wide range should not be regarded as normal, or safe, in pregnancy, and that levels below 2.5 mIU/L in the fist trimester should be maintained by increased supplementation with thyroid replacement therapy. (7)
Because the risks for pregnancy loss are greatest during the first trimester, TSH evaluations should ideally be performed well in advance of the first antenatal visit, both to provide a TSH baseline, and also to assess any TSH increases in the 2nd and 3rd trimester, and postpartum period.
It would be an act of gross negligence by a medical practitioner to ignore the TSH levels of his pregnant patient and to withhold thyroid replacement therapy as demanded by an elevation of TSH in early pregnancy.
Sadly, many cases of pregnancy loss have been reported, where TSH levels have been ignored and additional thyroid hormone has not been provided for the needs of the growing feteus.
The American Thyroid Association (ATA) recommends the following ranges for TSH during pregnancy :
First Trimester: (0-13 weeks) 0.1 – 2.5 mIU/L.
Second Trimester (14-26 weeks) 0.2 – 3.0 mIU/L
Third Trimester (27-40 weeks) 0.3 – 3.0 mIU/L
The 2007 Endocrine Society Clinical Guidelines are in agreement with these ranges, calling for hormone replacement medication to be adjusted during pregnancy, to maintain a TSH level not higher than 2.5 mIU/L prior to pregnancy, and less than 2.5 mIU/L in the first trimester, and 3.0 mIU/L in the second and third trimester. (8)
Any increases in TSH beyond these recommended levels will necessitate an appropriate increase of up to 50% of the current thyroid hormone replacement therapy.
In a study of pregnant women where pregnancy outcomes in 2 groups were compared, each with different levels of TSH, the group with TSH levels below 2.5 mIU/L recorded a pregnancy loss of 3.6%, while the group with a higher TSH of 2.5-5.0 mIU/L recorded a pregnancy loss of 6.1%.
On the basis of these results the risk of miscarriage increased by 15% for every 1 mIU/L elevation of TSH. (9)
In cases where pregnant women had detected levels of Thyroid antibodies (Hashimotos Thyroiditis) their risk for pregnancy loss was doubled, indicating the importance of screening for thyroid antibodies well in advance of the first pregnancy visit. (10)
Many cases of subclinical hypothyroidism are missed because of reported “normal” Thyroid levels and only slightly elevated TSH levels, despite the complaints to their doctors that the patients involved are chronically fatigued, or plagued by additional symptoms of mental fog, muscle pain, and inability to lose weight.
In these cases the presenting symptoms have greater significance than the reported lab results, and these patients may require thyroid replacement therapy before feeling better, despite the “normal” appearance of their blood hormone levels.
POST PARTUM THYROID DYSFUNCTION (PPTD)
Post-partum thyroid dysfunction may occur in 50% of females where thyroid antibody levels (TPO) were elevated in early pregnancy (Hashimoto’s Thyroiditis). In these cases thyroid replacement therapy must be maintained during this period since 25%-30% of these females may develop permanent hypothyroidism. (11)
(7) GRAVES DISEASE: (Hyperthyroidism)
Hyperthyroidism also presents a risk to pregnancy, where abnormally high levels of thyroid hormone can lead to premature birth or pre-ecclampsia, with dangerously high levels of maternal blood pressure and risk of seizure and fetal death.
Symptoms of Graves are a rapid pulse rate and heart rate, with increased blood pressure and body temperature, restlessness, tremor and ultimately a “thyroid storm” which will require emergency medical treatment
The medical treatment during early pregnancy is with propylthiouracil (PTU), followed later by methimazole, which should be avoided during the first trimester.
(8) Replacement Thyroid Hormones :
The standard thyroid hormone replacement used by most doctors is sodium thyroxine (Levothyroxine), which is a synthetic preparation of T4, while natural dessicated thyroid hormone preparations (NDT) are also available, providing both thyroxine (T4) and triiodine (T3) in combinations of varying strengths.
Some patients do better taking bio-identical hormones, such as Naturethroid, (or NP Throid and Westhroid) a dried extract of pig thyroid gland, which is a mix of T4 and T3.
(The use of natural thyroid extract goes back many years, long before the synthetic hormones became available. Most practicing doctors are only familiar with the more recent synthetic variants popularized by the pharmaceutical industry.)
Many patients who have been diagnosed as hypothyroidism, or having Hashimoto’s Thyroiditis, and treated by their doctors with Levothyroxine, continue to feel unwell, complaining of chronic fatigue, mental fog, muscle pains, hair loss, cold extremeties, and constipation, despite their prescribed medication, and often having hormone levels which fall within the “normal” reference range.
While their Thyroid medication serves to effectively suppress their TSH levels, giving an impression that they are being adequately managed, with a TSH that is “within the normal range”, they remain unwell, and invariably raise health concerns that their doctors are often unable, or unwilling, to address.
This situation presents a dilemma for many doctors, who have little else to offer, other than a recommendation for antidepressant therapy, or referral to a psychiatrist.
Astute patients know that they are not depressed, and many have reportedly refused treatment for depression, prompting them to look for answers elsewhere.
An underlying problem in many of these cases may be T3 deficiency, caused by failure of T4 conversion to the biologically active T3.
This failure may be the result of nutrient deficiencies, or any one or more of the deiodinase enzymes.
(9) The Deiodinase Enzyme System :
The interplay between the deiodinase enzymes and the thyroid hormones can be quite complex, and the reader is not required to understand the details of the conversion process, other than to recognize that these conversions do occur, and failure to convert T4 to T3 may, in some patients, be the underlying cause why they fail to feel better, despite the conventional treatment with standard medication, like thyroxine, which is primarily T4.
The deiodinase enzymes have a crucial role to play in controlling the levels of thyroid hormones in the brain, and together they perform a balancing act that protects the brain from the destructive effects of hypothyroidism and hypothyroidism.
The 3 deiodinase enzymes, D1, D2 and D3, have distinctive areas and mode of operation, with D1 involved in the conversion of T4 to T3 in the liver, and D2 enabling the conversion of T4 to T3 in the brain astrocytes, where 80% of the thyroid hormone is in the form of T3, and 20% in the form of T4.
Enzyme D3 is selectively expressed in neurones (nerve cells), where it inactivates both T4 and T3, and converts them into T2, and a storage thyroid called reverse T3 (RT3), so that when thyroid hormone levels are low, D2 is expressed to produce T3 in the astrocytes, and when thyroid levels are too high, D3 is activated, which degrades both T4 and T3 and converts these hormones into T2 and reverse T3 (RT3).
The deiodinase enzymes, while active in the brain astrocytes and neurones, are also widely distributed in other parts of the body, such as the thyroid itself, and pituitary gland, and also in muscles, liver and kidney. (12)
Some patients appear to have a defective deiodinase gene, which prevents the peripheral conversion of T4 into T3, rendering them dependent on T3 supplementation.
For these people medication with standard Thyroxine or Synthroid (T4) does not satisfy the body’s requirement for T3, resulting in the persistence or worsening of their symptoms, until they are given T3 (Cytomel) or a T3/T4 combination such as Naturethroid, or other similar natural dessicated thyroid hormones (NDT).
In these cases levels of blood T3 should be carefully monitored, with low levels of T3 be given to start with, and slowly increasing to a level where symptoms are relieved, and palpitations are avoided from an excess of T3.
A starting dose for T3 should be low, often at one half grain (32.5 mg), with slow increments under the supervision of a medical practitioner who is familiar with thyroid hormone supplementation, and a review of TSH, T3, T4 and RT3 at 4-8 week intervals, before dose adjustments are made.
In most cases of levothyroxine therapy lab results, both in the pregnant and non pregnant state, will return to normal and symptoms may be resolved, but a subgroup of patients may reflect anomalous thyroid function levels which can be a source of frustration and confusion, both for patients and clinicians alike.
These cases may require more detailed investigation followed by specialized medical management, since non-thyroid illness (NTI), such as malnutrition, sepsis, burns, malignancy, myocardial infarction, chronic liver and renal disease, may alter T3 and TSH within 24 hours.
(10) Reverse T3 (RT3) :
Reverse T3 (RT3) is a metabolite of T4 (Thyroxine). Under conditions of stress the body conserves energy by converting T4 to RT3.
T4 can also be converted to T3, through the loss of one iodine atom (monodeiodination).
RT3 differs from T3 in the position of the iodine atoms attached to the aromatic ring, and is the inactive form of T3, serving to hold thyroid hormone in reserve to allow the body to overcome the burden of stress.
Elevated levels of RT3 may signal a state of hypothyroidism, even though TSH, free T3 and free T4 are within the normal range.
The Mayo Clinic records a reference range of RT3 as being 10-24 mg/dl.
A ratio of FTR: RT3 = 20 or higher suggests a safe value for RT3, and higher than this may signal a problem.
Elevated RT3 may reflect increased adrenal dysfunction arising from prolonged stress, and may also indicate an elevation of cortisol as well as a drop in cortisol levels, also indicating conditions of stress.
Under conditions of body stress the normal conversion of T4 to T3 favours the conversion of T4 to RT3, as a means of energy conservation.
The RT3 level may tend to follow the T4 level, and be low in hypothyroidism and high in hyperthyroidism.
Reverse T3 is selectively expressed by Deiodinase 3 to deactivate both T4 and T3 when neurones require protection from an excess of thyroid hormones.
Under normal conditions intracellular conversion of T4 to T3 takes place in the brain astrocytes under the action of deiodinase 2 (D2), producing 80% of T3 (9).
During periods of physical or emotional stress thyroid hormones T3 and T4 may be converted into reverse T3 (RT3) to conserve energy. Cortisol levels would increase under these conditions of stress, with RT3 levels increasing, thereby inhibiting the conversion of T4 to T3, so that more T4 is converted into RT3 for storage.
While T4 may be considered the storage hormone, and T3 the energy hormone, RT3 may be considered to be the emergency brake when excess T3 is being produced.
Too much T4 being produced by an overactive thyroid can cause hyperthyroidism, so excess T4 is converted into RT3 as a protective mechanism.
Too much RT3 will compete with the T3 receptor site and block the peripheral uptake of T3, a process which occurs in times of stress, causing an increase in blood levels of T3 rather than in the cells.
An elevation of RT3 may then be treated with low dose increments of T3, at about 5mcg to 10 mcg 2-3 times daily. To maintain a RT3: T3 ratio of greater than 20.
A lower ratio may signal too much RT3 and a sign of underlying stress.
Some researchers state that a level of RT3 will always be present in the blood, but too much will block T3 receptor sites and should therefore be reduced by attending to stress factors, which may be an underlying cause of RT3 excess.
An excess of RT3 may reflect high levels of T4, and a TSH which is within the normal reference range, giving the false impression of a normal functioning thyroid, and no need for treatment.
While inflammatory demands of any cause can lead to an increase of RT3, low levels of iron may also result in an increase in T4, with excess T4 being converted into RT3.
An excess of RT3 may result in “pooling” of T3 in the blood due to competition with T3 at the receptor site, leading to high circulatory levels of T3, resulting in symptoms of anxiety or palpitations, which should not be interpreted as being a state of hyperthyroidism.
A good RT3 level is under 15, with an ideal level being 10-24 mg/dl. (Mayo Clinic).
It has been suggested that the T3:RT3 ratio is the most useful marker for tissue hypothyroidism and as a marker of diminished cellular functioning. (13)
These researchers suggest that TSH and T4 as markers for hypothyroidism are ineffective, because they do not reflect the activity of the biologically active thyroid hormones at cellular level.
(11) Inflammation and Thyroid Disorders :
One common form of hypothyroidism is Hashimoto’s Thyroiditis, which is a disorder of inflammation, in which inflammatory proteins adversely affect the actions of the deiodinase enzymes, with reductions in thyroid hormone levels.
Other causes of hypothyroidism are surgical removal of part or all of the thyroid, radio-active iodine treatment for an overactive thyroid, treatment of Pituitary tumours, congenital birth defects and some drugs, like Amioderone and Lithium.
Inflammation can lower D1 activity, which compromises the conversion of T4 to T3, reducing the availability of T3 to peripheral cells.
Raised CRP levels are an indicator of underlying inflammation, and may decrease cellular T3 levels, without being detected by normal thyroid testing, but elevate pituitary T3 resulting in lowering of TSH, and giving the appearance of “normal” thyroid testing.
Pregnant and non pregnant patients with Hashimoto’s Thyroiditis may benefit from nutritional support which includes Turmeric, Ginger, Resveratrol, Glutathione, Zinc, Selenium and vitamin D3, and elimination of food that can cause inflammation, such as gluten, soy, dairy, sugar, processed foods and foods with chemical additives.
Some texts refute claims for Thyroid benefit from minerals like zinc and selenium, ignoring the evidence that Selenium is a co-factor in the enzyme 5’ deoidinase which aids the conversion of T4 into T3, while also degrading reverse T3 (RT3) (14), and zinc can support the elevation of T3. (15) (16)
Glutathione is a powerful antioxidant that is able to neutralize many harmful free radicles and detoxify toxic metals, chemicals and carcinogens that present a threat to normal thyroid function. (17) (18).
Glutathione, is dependent on NADP for its conversion to the active form (GSH), and NADP plays an important role in the conversion of T4 to T3.
The nutrients required for Glutathione synthesis are Vitamin B6, P-5P, B12, Zinc, magnesium and selenium.
Poor dietary Iron intake has also been implicated as a causal factor in hypothyroidism, with ferritin stores serving as an indicator of adequate or inadequate levels of iron.
These nutrients are safe in pregnancy, and may aid in the restoration of thyroid function where inflammation has resulted from stress or from nutritional deficiencies or dietary indiscretions.
Dr. Neville Wilson.
www.drnevillewilson.com
000000000
REFERENCES :
- Cell Mol Life Sci (2008) 65:570-90)
- Endocrinology (2009) 150; 1097-197.
- Best Pract Clin Endocrinol Metab 201§3; 27(6):745-762 Koulari O, et al.
- J Clin Endocrinol Metab. 2007; 92:S1-S47
- Irish Med Journal 2013; 106(4): 107-116, Khalid, AS.
- J Autoimmun 2013,38,J275-81
- JAMA 2004; 291-228, Surks MI et al.
- J of Clinical Endocrinology and Metabolism 2007, 92(8) (Supp):S1-S47.
- JAMA 2004;291:228-238, Surks MI et al.
- J Clin Endocrinol Metab 2007; 92:S1-S47
- J Clin Endocrinol Metab 2011, Mar, 96(3): 614-6, Lazarus H.
- J Clin Endocrinol Metab 2009; 94(5):1623-1629
- J of Clinical Endocrin & Metab 2005;90(12): 6403-9, Annewieke W et al.
- AMJ Clin Nutr 1993
- Horm Metals Res 1996
- Biol Trace Elements Res 1996.
- Endocrinol Journal 1980 (Apr; 27(2);201-7.
- Int J Toxicol 2001 Jan-Feb; 20(1):15-20.
0000000000000000000000


Hi! I am trying to conceive and I am using Lugol’s Iodine Solution 5%, two drops per day. There is some differente TSH parameters for Lugol’s users? Thank you very much.
Thank you for this article and information. It is really refreshing to see a GP in Ireland who looks at the whole issue of thyroid disease, and not just the quick solution of medication. I have read a book by Izabella Wentz, PharmD. FASCP. She also looks at treating and if possible reversing thyroid disorders through dietary changes, supplementation and bio-identical hormones if needed. I suffer with Hashimoto’s (but I am not completely symptom free thanks to lifestyle & dietary changes) and working on reducing my medication. Thank you again for the great information in the article, very helpful.
typo *(but I am NOW completely symptom free thanks to lifestyle & dietary changes)
Hello..
Can someone guide me please.
I’m in Eltroxin over 3 years now and I’m looking to come off them. I was recommended to Dr Wilson by one of his patients.
Could someone point me in the right direction so I can make an appointment!
Thank you
Fal