by DR. NEVILLE WILSON.
PREAMBLE:
Coronary Heart Disease (CHD) remains the leading cause of death in the Western World. Yet, despite the documented decrease in cardiac-related mortality since the late 1960s, the incidence of CHD has not declined in recent years. (1)
Data from EUROASPIRE III shows that primary strategies for cardiovascular risk reduction have not been successful, raising questions about current intervention policies and practices. (2)
It is therefore timely and appropriate to review the classical guidelines that dictate practice policy, taking account of new data recently extracted from previous studies.
Newly emergent data reveals a consistent pattern of associations between low levels of HIGH DENSITY LIPOPROTEIN-CHOLESTEROL (HDL-C) and an increased risk of CHD.
This paper reviews emergent data that demonstrates the cardiovascular benefits of a high level of HDL-C, and examines the nature and properties of HDL-C, followed by references to possible strategies for improving HDL-C levels for purposes of reducing the risk of CHD.
NCEP RECOMMENDATIONS:
In 2004 the National Cholesterol Education Programme (NCEP) recommended reductions of low density lipoprotein cholesterol (LDL-C) to targets of 2.6 mMol/L (<100mg/dl) as a strategy for reducing the risk cardiovascular disease, and even to lower targets of 1.81mMol/L (<70mg/dl) in high risk patients. However, this strategy has failed to produce the expected levels of benefit, as shown by current reviews of the evidence, thereby prompting an ongoing search for an optimal atherogenic lipid risk profile that is predictable and measurable.(3)
Epidemiological studies have uncovered an association between low high density lipoprotein (HDL-C) and an increased risk of CHD, thereby identifying a potentially important area for cardio – protection intervention. These findings give credence to the hypothesis that HDL-C levels provide greater predictive value for cardiovascular risk than do LDL-C levels.
This hypothesis is currently the focal point of much research in endeavours to profitably identify the significant factors that contribute to morbidity and mortality risk.
FRAMINGHAM STUDY:
Data from the Framingham Study as far back as 1977 showed that HDL-C was a more potent predictive factor for risk than LDL-C. (4) In 12 years of follow-up for 2748 participants, aged 30 – 79 years, low levels of HDL-C were associated with increased mortality. ( 5) Despite this revelation, LDL-C reduction with statin therapy remains the focus for risk management initiatives in current guidelines.
The NCEP guidelines also state that “setting a specific goal value for raising HDL-C was not warranted”. However, it is evident that while statin drugs can effect marked LDL-C reductions, their capacity to raise HDL-C is limited to 3% -15% or is absent. (6)
TNT STUDY. (TO NEW TARGETS).
New data from the TNT Study reveals that subjects who had their LDL-C levels substantially reduced with high dose (80mg) Lipitor, nevertheless remained at risk if their HDL-C levels remained low. Prof. Philip Barter and colleagues showed that a low level of HDL-C remains predictive for major cardiovascular events, even in statin treated patients who have achieved low LDL-C levels of below 70mg/dl (1.8Mm/L). (7).
The TNT STUDY sought to test the risk benefits of lowering LDL-C to new targets and selectively investigated 1001 patients with stable CHD, who were randomized to either 80 mg Lipitor or 10 mg Lipitor per day, and followed for 4.9 years. (Of the original 18,469 participants screened for inclusion in the study 8468 were excluded for a variety of reasons, some not stated.)
The TNT STUDY researchers reported a “significant risk reduction of 22%, prompting declarations from some quarters that “lower is better”, with reference to LDL-C targets. The apparently “significant” benefits of 22% looked less impressive when the absolute risk reduction revealed an insignificant benefit, prompting several observers to call for caution with respect to LDL-C lowering.
Newly obtained data from TNT now clearly shows that those subjects who had low LDL-C levels, irrespective of the degree to which their LDL-C had been lowered while taking high dose Lipitor, nevertheless remained at risk for a major cardiovascular event. (7)
In TNT 2661 of the subjects achieved the desired low levels of LDL-C (1.8mMol/L: <70 mg/dl) and yet remained at significant risk. Those with HDL-C levels >55mg/dl (>1.42 mMol/L ) had a 39% lower risk of a major cardiovascular event than those with HDL-C levels of <37 mg/dl (0.96 mMol/L).
The concept that “ lower is better” has thus been overshadowed by an emergent awareness that “higher is better “, thus demonstrating the limitations of current guidelines, and the need to incorporate HDL-C as an important therapeutic target.
THE PROCAM STUDY:
Procam Study researchers analysed data from more than 20,000 subjects in Germany over a period of 25 years and developed a scoring system for predicting global CHD risk. Unlike the homogenous American population targeted by the Framingham investigators, a Northern European population was selectively studied between 1979 and 1995. This study showed that HDL-C is an important driver of CHD risk, and provided evidence that HDL-C levels exert a much stronger influence on CHD risk in individuals with elevated global risk. An important outcome of Procam was that CHD risk factors do not act in isolation, but in conjunction with each other. (8).
MAJOR STUDIES REVIEWED:
A review of the data from three major studies (a) Lipid Research Clinics Prevalence (LRC) Mortality Follow Up, (b) Coronary Primary Prevention Trial (CPPT), and (c) Multiple Risk Factor Intervention Trial (MRFIT) revealed that every decrease in HDL-C level by 1 mg/dl (0.03mMol/L) was associated with an increase in the risk of CHD of 2% for males and 3% for females, confirming the evidence that emerged from earlier studies. (9)
Data from the HONOLULU HEART PROGRAMME indicated that higher levels of HDL-C ( up to 1.5 mMol/L (or 60mg/dl) should be attained to achieve risk containment benefit, and a review of the INTERHEART ASIAN STUDY data base revealed that subjects with normal or higher HDL-C had a lower risk of acute myocardial infarction (AMI) at all levels of LDL-C. (10) and that the ratio of ApoB/ ApoA1 was the strongest predictor of AMI risk in Asians.
INTERVENTIVE STUDIES:
The strong association between HDL-C and risk reduction, as evident in epidemiological studies, has also been tested in several interventive and experimental studies. (11)
Peter Libbey et al show that in all the major statin interventive trials the treated subjects have remained at risk despite their lowered LDL-C levels. (12) And in a meta-analysis of 90,000 subjects in 14 prospective randomised statin trials, low HDL-C at baseline represented a significant contributor to cardiovascular risk. (13)
The VETERANS AFFAIRS HDL INTERVENTIVE TRIAL successfully tested the hypothesis that raising HDL-C with a fibrate could produce benefits for high risk males, (14) thereby reproducing similar findings that emerged from the earlier HELSINKI HEART STUDY.
ApoA-Imilano (apoA-IM)
Carriers of the apoA-IM, a genetic variant of apoA-I, have extremely low levels of HDL-C, but have little evidence of cardiovascular disease. Intravenous infusions of recombinant apoA-IM induced a marked reversal of atherosclerosis in 57 patients with acute coronary syndrome (ACS) and >20% coronary artery obstruction, a study that has prompted cautious suggestions in some quarters of a future role for HDL-C infusions in high risk subjects. (16)
THE NATURE OF HDL-C:
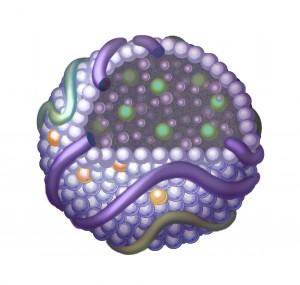
HDL-C is one of several groups of lipoproteins which facilitates the transport of lipids, including cholesterol and triglycerides, through the circulating blood stream. HDL is the smallest of these (7-12 nm diam.) and thus the most dense, containing the highest amount of protein.
Their composite and complex structure renders them capable of numerous biological functions. In addition to lipid transport mechanisms, they exhibit anti-inflammatory and anti-oxidant properties, thereby conferring a range of cardiovascular and cardioprotective benefits if sufficiently present.
HDL-C particles are constantly altering their shape and function, during which process they transport several types of phosopholipids and proteins in the plasma. While the core of the HDL-C particle is cholesterol ester and triglyceride (TG), its surface is comprised of phospholipids, free cholesterol and apolipoproteins, of which apo A-I appears to be the major surface protein.
HDL particles may be classified according to their (i) apolipoprotein, (ii) size, (iii) surface charge, (iv) density, thus a variety of designations may be used to describe the range of HDL-C particles so far identified. The two major sub fractions are HDL2 (large) and HDL3 (small), and these can be further allocated to sub populations, a, b, or c. HDL2b are the largest fractions (35% protein/65% lipids) while the HDL3c are the smallest fractions (65% protein 35% lipids). Small, dense HDL3 possesses multiple anti-atherogenic properties, including potent cholesterol efflux capacity and anti-oxidative, anti-inflammatory and anti-poptotic activities. (17)
The widespread and simplistic notion of LDL-C “clogging” arterial walls and HDL-C “scouring” these walls to “unblock cholesterol plugs”, ignores the complex sequence of inflammatory events that occur in the layers of the arterial wall during the process of atheroma formation. The concept of “bad cholesterol” plugging arteries while “good cholesterol” does the “unplugging” is unscientific and erroneous.
HDL-C exerts its beneficial influence by interfering with the process of vascular wall inflammation, and is operative at several levels in the cascade of events that leads to atheroma and plaque formation.
ARTERIAL WALL INFLAMMATION appears to be a “response to injury”, (18) following endothelial (arterial wall inner lining) damage from any of several factors which appear to play a pro-oxidant role in the process. There is no evidence that total cholesterol or LDL cholesterol (“bad cholesterol”) “causes” atherosclerosis . Alterations to native LDL-C may occur under pro-oxidant conditions giving rise to oxidized LDL which may initiate or aggravate an inflammatory process within the arterial wall, causing atheroma formation. HDL-C has been shown to interrupt this process in a beneficial way through the import of its anti-atherogenic properties.
THE ANTI-ATHEROGENIC PROPERTIES OF HDL-C:
1. INHIBITION OF MONOCYTE ADHESION:
Native LDL-C may be modified under certain adverse conditions, thereby stimulating the endothelial cells lining the arterial lumen to express a protein, monocyte chemotactic protein 1(MCP-1), which in turn attracts monocytes from the blood into the arterial wall. The oxidized LDL also causes the differentiation of monocytes into macrophages which engulf the modified LDL giving rise to the formation of foam cells. Macrophages also express cytokines which include tumour necrosis factor alpha (TNF alpha) and Interleuken-1, which cause the endothelial cells to express adhesion molecules E.selectin, Vcam-1, and Icam-1. These adhesion molecules bind the monocytes to the endothelium, and some of them are attracted into the artery wall by MCP-1.
HDL intercepts this inflammatory process by inhibiting the expression of E selectin and
Vcam-1, thereby decreasing the binding of inflammatory cells within the arterial wall
inhibiting the process of atherosclerosis. (19)
2. INHIBITION OF LDL-C OXIDATION.
HDL contains an enzyme, Paroxinase 1 (PON 1), which inhibits the formation of MCP-1, thereby preventing its attraction into the arterial wall. (20). It also protects LDL from oxidation, limiting thereby the inflammatory response to modified LDL. By preventing the oxidation of LDL, via PON 1, HDL inhibits the vasoconstricting effects of oxidized LDL, effected through Nitric Oxide depletion. It thus permits vasodilation and improves endothelial function.
HDL also carries alpha- tocopherol (vit.E) to the endothelial cells thereby providing another mechanism for suppressing the oxidation of LDL. Vitamin E inhibits the ability of oxidized LDL-C to induce 1CAM-1 expression, (21) and has also been shown to suppress the gene that codes for 1CAM-1. (22)
High levels of vitamin C have also been shown to be associated with high plasma HDL and HDL2, suggesting that high plasma levels of vitamin C may lower atherogenic risk by increasing HDL-C. (23)
The Flavenoid Quercetin, has also been shown to enhance the protective mechanisms of HDL-C by upregulating PON1 gene expression and its protective capacity against LDL-C oxidation. (24)
3. ANTI-THROMBOTIC PROPERTIES OF HDL-C
Intra-arterial thrombi may occlude vessels and lead to cardiovascular or cerebro-vascular
events, and are dependent on the degree of plasma coagulation, which in turn is determined,
either, by reduced fibrinolysis or increased platelet aggregation.
Since levels of tissue plasminogen activator (PAI-1) determine the fibrinolytic capacity of the
blood, conditions which predispose to elevated PAI-1 would represent risks to health.
Low levels of HDL-C have been shown to correlate with elevated levels of PAI-1, (25) and in a study of males without a history of cardiovascular disease, Halle et al correlated hyperfibrinoginaemia with elevated levels of LDL and reduced levels of HDL2. (26)
Therefore, HDLs exert anti-atherogenic and anti-thrombotic effects that are consistent with a marked reduction in the risk of cardiovascular morbidity or mortality.
These findings support the use of preventative or therapeutic strategies to improve HDL levels in subjects who are at risk by virtue of having low HDL levels.
4. REVERSE TRANSPORT:
HDL is capable of transporting cholesterol from peripheral cells to the liver for recycling and excretion into the bile. Under the action of the enzyme lecithin-cholesterol acyl transferase (LCAT) free cholesterol is converted into cholesterol ester, which is more hydrophobic, and then sequestered into the core of the lipo- protein particle, which becomes larger as more cholesterol is incorporated.
The cholesterol is then delivered to the liver, or to the steroidogenic organs, such as the adrenals, ovary, or testes, where it is beneficially utilized in the production of steroid hormones. One of several pathways is an indirect one, mediated by cholesterol ester tranferase protein (CETP) in which cholesterol is transported from lipid laden macrophages.
CETP also facilitates the transfer of cholesterol from HDL particles to the VLDL/LDL in exchange for triglyceride, thereby reducing circulating HDL levels. This process may be pro-atherogenic since cholesterol is delivered from the protective HDL to the pro-atherogenic VLDL/LDL and is itself reduced quantitatively in the process.
It becomes evident then, that both LDL-C and HDL-C can be modified under certain physiological conditions to become pro-atherogenic.
The pharmacological inhibition of CETP continues to be explored as an option for raising HDL levels, despite the earlier unfortunate consequences of CEPT inhibition by the drug Torcetrapib. (Illuminate Study).
THE PREVALENCE OF LOW HDL-C:
Data from the NHANES data base over a 30-year period (1976-1980); (1988-1994); (1999-2006) reveals a prevalence of low HDL-C and a concomitant doubling of triglyceride (TG) between 1999-2006 (from 2.1% – 4.8%) and a trebling from 1.8% – 8.7% between 1976 and 2006. (27)
Accompanying these changes in HDL-C and TG is a trend of escalating obesity, which has more than doubled (15% – 33.7%) between 1976 and 2006. Escalating rates of obesity are prevalent at a time when low fat / high carbohydrate diets are encouraged and endorsed by the food and health industries. The American Heart Association (AHA) recommends low-fat diets, thereby encouraging consumers to replace these dietary options with processed foods that are low in saturated fat, high in simple carbohydrates and high in trans-fatty acids.
THE HEALTH BENEFITS OF HIGH HDL-C
Scant recognition is given to the fact that dietary saturated fats, in fact, raise HDL levels and improve lipid ratios, (28) and have been shown to reduce the progression of coronary artery disease in post-menopausal women. (29) ( These facts have been known for a long time, and were reported in an analytical review of 27 studies in 1992, (30) and only referred to in 2000 by the American Heart Association in its revised dietary guidelines. )
The dietary intake of the anti-oxidants vitamin E and vitamin C also raise HDL-C levels, as does resveretrol, a poly-phenol component of red grape skins and seeds, thereby imparting cardio-protective benefits.
Since aerobic exercise also raises HDL-C, a sedentary lifestyle, coupled with the consumption of simple carbohydrates at the expense of complex carbohydrates and healthy fats, inevitably contributes to elevated triglycerides and low HDL levels, and thereby increases the risk of morbidity and mortality.
STRATEGIES FOR INCREASING HDL-C LEVELS:
Interventive strategies for raising healthy HDL-C levels will include lifestyle changes that incorporate the following:
(i) Body weight reductions through calorie restriction. For every 1 kg. of body weight reduction there is up to 1% increase in plasma HDL-C, if weight loss is sustained.
(ii) Aerobic exercise has been shown to raise HDL-C by about 3%. Moderate exercise several times a week has also been shown to be effective for this purpose.
(iii) Smoking can reduce HDL-C, while smoking cessation can increase HDL-C by as much as 10%.
(iv) Moderate alcohol consumption can increase HDL-C, but may also increase the levels of potentially atherogenic lipo-proteins and triglycerides, which may counteract any potential benefits associated with HDL-C increases. Resveretrol, a polyphenol present in the skins and seeds of red grapes, improves HDL-C levels favourably.
(v) Dietary saturated fats can raise HDL-C levels. Contrary to the recommendations of the American Heart Association (AHA), many lipid researchers advocate the inclusion of healthy saturated fats, such as lauric acid and myristic acid, in the daily diet and the exclusion of harmful trans-fats which are ubiquitious in processed foods. (31)
(vi) Omega 3 polyunsaturated fats favourably influence plasma lipids providing an improvement in immune status in a dietary intake ratio of 3;1 (omega 6/ omega 3), and may be obtained from cold water oily fish (salmon) or quality fish oil supplements. An excess of omega 6, as found in a typical western diet, of 20:1, may shift the physiological state to pro-inflammatory. (32)
(vii) The dietary or supplemental role of the anti-oxidants vitamin E, vitamin C and Quercetin have a supportive role in maintaining healthy levels of HDL-C.
While pharmaceutical agents for raising HDL levels are available, sole reliance on these mechanisms for cardiovascular risk reduction are likely to impede progress in the education process aimed at effecting beneficial lifestyle modifications.
Fibrates have been shown to increase HDL-C by 10%, and Nicotinic Acid can achieve HDL-C increases of up to 30% and reduce triglycerides (Tg) by 40% to 50%, and reduce LDL-C by up to 20%.
CETP blockade can increase HDL-C by as much as 50%, but the potential role of CETP inhibitors has been called into question following termination of the ILLUMINATE study.
Anacetrapib is a CETP inhibitor currently under clinical investigation, and appears not to be associated with blood pressure increases, as was Torcetrapib. At 10mg. It has shown increases of HDL-C up to 41%.
JTT-705 is another CETP inhibitor that raises HDL-C without evidence, so far, of blood pressure increases.
Combination therapy of ER Niacin and simvastatin are being evaluated in the AIM-HIGH STUDY.
Ongoing intervention studies will further define the benefits of combination therapies that reduce LDL-C and elevate HDL-C.
.
Strategies for raising public awareness of risks to health remain the responsibility of primary care physicians who are best placed to advocate drug free options before resorting to prescription medicines.
The INTERHEART STUDY results indicate that a multiplicity of factors are likely to be implicated in cardio-vascular disease, and that psycho-social factors, may contribute to a substantial proportion of the risk for acute myocardial infarction. (AMI)
While the global effect was less than for smoking, it was comparable with hypertension and obesity. The effects of stress on AMI were similar in men and women, in people of all ages, and in all geographic regions of the world studied.
CONCLUSION
The INTERHEART STUDY reminds us that the risks to health are multi-factorial and that multi-level interventions may be required to reduce the levels of risk for many people. These should include strategies which prioritise lifestyle changes. A preoccupation with lipids while ignoring other vital factors that impact on cardiovascular health will do little to stem the tide of an escalating and seemingly unstoppable trend.
Healthy lipid ratios, rather than lipid levels, remain part of the global target for cardio-vascular disease risk reduction. Since current preoccupations with LDL-C and total cholesterol (TC) lowering have not succeeded in attaining such desirable objectives, the shift to a newparadigm that embraces HDL-C enhancement is incumbent.
DR. NEVILLE WILSON.
APRIL, 2009.
REFERENCES:
2. Eur J. Cardiovascular Prev. Rehab 2009.
3. Am J. Cardiol. 2006,Feb., 1:97(3):372-5
4. A. Med. J 1977;62:707-14 Framingham Study.
5. Arteriosclerosis, Thrombosis & Vascular Biol. 1988:8;737-741
6. Am Coll of Cardiol Annual Sc. Session, Orlando, March,29-31, 2009-05-03
7. NEJM. Vol. 357, Sept 27, 2007;1301-1310
8. Atherosclerosis 1996;124 Supplement:S11-S20
9. Circulation:1989; 79: 8-15
10. Lancet 2004; 364:937-52
11. J Am Cardiol 2008; 51:49-55
12. J Am Coll Cardiol: 2005; 46:1225-8
13. Lancet 2005; 366:1267-78
14. JAMA 2110; 285; 1585-1591
15. Nejm 1987: 317:1237-1245
16. JAMA 2003: 290; 2292-2300
17. Nat Clin Pract Cardiovasc Med. 2006: 3(3): 144-153
18. Am J Pathol 1977 March, 86(3): 675-684
19. European Heart J Supplements, vol 7, supp F-Philip Barter.
20. Biochem Biophys Ref Comm 2004; 318:680-683
21. Bejing Da Xua Bao, 2004, Feb 36(1):70-74
22. Ann NY Acad. Sci 2004 Dec; 1031:86-95
23. Am J Clinical Nutrition 1994 July: 60(1):100-5
24. Biochem & Biophysical Research Communications vol 379, issue 4, 20 Feb.2009 (p.1001-4)
25. Thrombo Res 1993:70:161-171
26. Arteriosis, Thrombosis and Vascular Biology, 1996: 16; 144-148
27. NHANES: Circ 2008; 118:S_1081-S_1082
28. J. Nutrition 133; 78-83, Jan 2003
29. Am J Clin Nutrition 2004,; 80:1175-84
30. Arteriosc Thromb 1992 Aug; 12 (8): 911-9
31. Know Your Fats: Mary G. Enig, Ph.D
32. Fats Are Good For You : Jon J. Kabara, Ph.D


One Reply to “HIGH DENSITY LIPOPROTEIN – HIGHER IS BETTER”