by Dr. Neville Wilson
30 Jan 2013
Tredaptive was introduced into the European drug market on 3rd July 2008, as a pharmaceutical formulation designed to treat certain forms of mixed dyslipidaemia in patients judged to be at risk of cardiovascular disease.
On the basis of well established cardiovascular benefits of nicotinic acid, Merck Sharp & Dohne Ltd. (MSD) formulated and marketed a combination of nicotinic acid (1000mg) and laropiprant (20mg), a prostaglandin (DP1) antagonist, selected for its anti-flushing property, an unwanted, yet harmless, adverse effect of nicotinic acid in some patients.
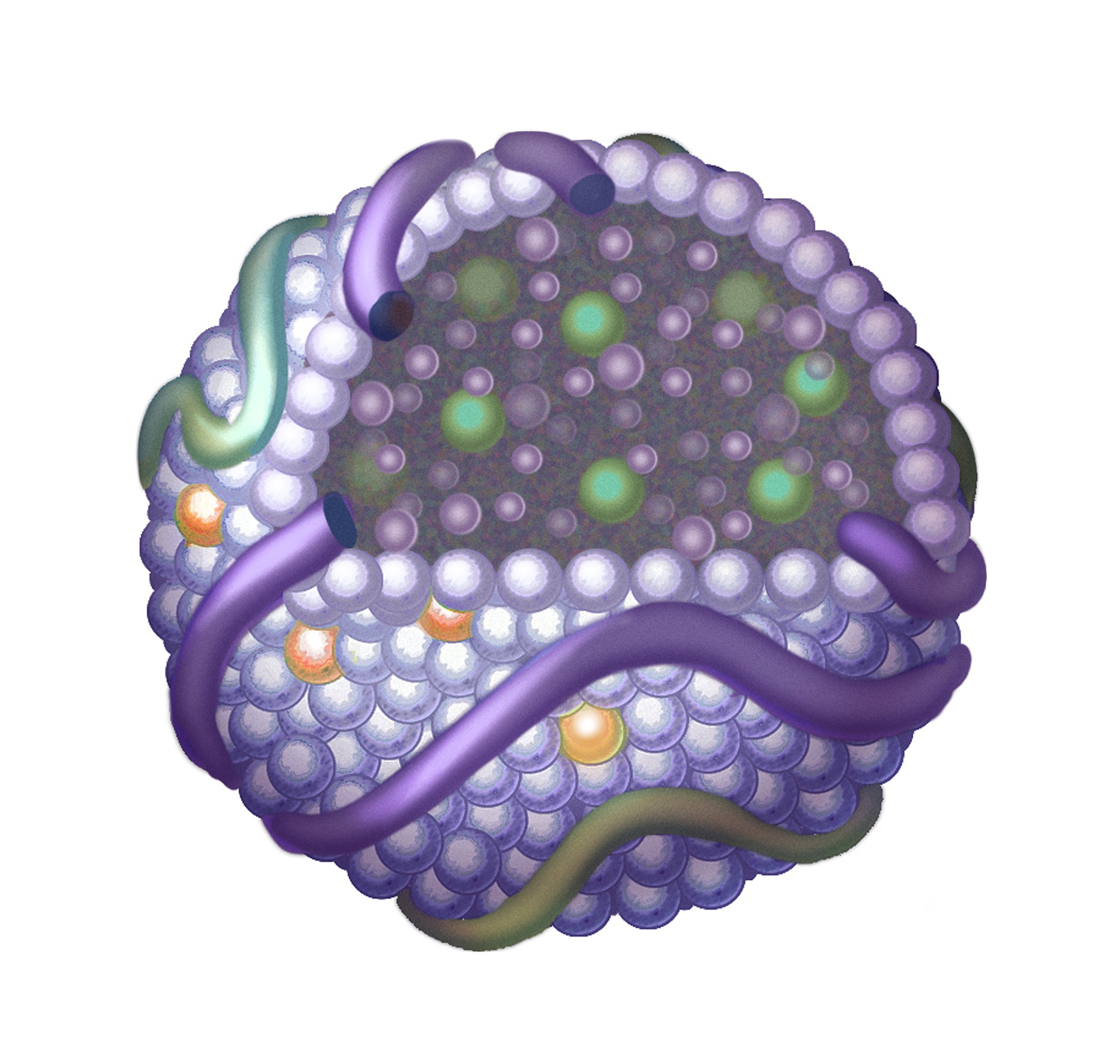
In combination, nicotinic acid and laropiprant (Rx TREDAPTIVE) achieved desirable lipoprotein ratios in dyslipidaemic patients, by raising HDL-C levels and lowering Triglyceride (Tg) levels in patients who were estimated to be at risk of cardiovascular disease.
HPS2-THRIVE:
In the recently concluded HPS2-THRIVE study, the combination of nicotinic acid / laropiprant (Tredaptive) failed to produce a statistically significant reduction in coronary deaths, non-fatal heart attacks, strokes or revascularization procedures, being the composite endpoint which the study was designed to assess. (1).
In the light of these findings, and their assessment by the Pharmacovigilance Risk Assessment Committee (PRAC) and the Committee for Human Medicinal Products (CHMP), the European Medicines Agency (EMA) have called for the suspension of TREDAPTIVE and the discontinuation of its use by clinicians as of 12nd January 2013.
The decision to discontinue the clinical use of TREDAPTIVE is unlikely to dissuade clinicians, who have traditionally used Niacin for purposes of raising HDL levels in selected patients, from continuing to do so. Their objective would be to raise low HDL levels in order to achieve the ideal ratio for Total cholesterol:HDL to be 4 or less.
The OTC formulation of Nicatinamide is suitable for such a strategy.
It may, on the other hand, provoke concerns amongst those clinicians who have not become familiar with the benefits of Niacin, and who will view the use of Niacin with caution, and thus withhold it’s use from deserving patients.
The pharmacological combination of Niacin (nicatinamide) and a prostaglandin (laropiprant) had not previously been tested for safety, and the further addition of a statin to this combination, as in HPS2-THRIVE, was destined to be of questionable efficacy and safety.
This raises critical questions about the design of HPS2-THRIVE.
It must be noted that the trial was not designed to answer whether or not raising HDL with nicatinamide affects risk, as low HDL was not an inclusion criterion.
Patients with low HDL-C werenot preselected, and all levels of HDL were represented in the treatment arm, making it difficult to evaluate the significance of HDL increases from a variable baseline level.
The benefit of raising a higher HDL level will not be as significant as raising a lower level of HDL.
The question asked of HPS2-THRIVE was whether nicotinamide, in combination with laropiprant, prevents vascular events in high risk patients who are already receiving intensive lowering treatment with a statin.
In many clinical scenarios TREDAPTIVE would have been given to at risk patients who were not receiving statins, and the conclusions of this study would not be applicable to such groups of patient.
THE STUDY DESIGN:
In HPS2-THRIVE 25,673 patents (14,741 in Europe and 10,932 in China) considered to be at high risk for cardiovascular events, were randomized to a placebo arm, in which patients were given a statin (simvastatin 40 mg or 1 tablet of ezetimibe 10 10mg/simvastatin 40mg ) for a background LDL lowering effect.
In the treatment arm patients were given 2 tablets of extended Niacin 1000mg / laropiprant 20mg (niacin 2000 mg + laropiprant 40mg ) plus simvastatin 40mg, or ezetimibe 10mg / simvastatin 40mg, in a single dose.
The question must therefore be asked, whether it was niacin, or laropiprant, or the inclusion of a low dose statin in the treatment group, and in the placebo group, or the off target effects of Ezetimibe, that caused the trial to fail in respect of safety and efficacy.
NIACIN BENEFITS:
In a meta-analysis of 11 studies including 9,959 subjects (including Arbiter-2, Arbiter-6 and AIM-HIGH) treatment with niacin on its own was associated with a significant 25% reduction in coronary heart disease events, and a significant 34% reduction in the composite endpoint of any cardiovascular disease. (2).
A review of recent randomized controlled trials have revealed a significant residual risk for cardiovascular disease events, even at low levels of LDL in the presence of low HDL levels, and this sizable residual risk has been diminished by augmenting HDL-C, for which niacin has a successful track record. (3) (4).
In addition to raising low HDL levels, as well as apolipoprotein-A1, in patients who are at risk, niacin has demonstrated reductions in total cholesterol (TC), triglycerides (Tg), very low density lipoprotein (VLDL) and lipoprotein a (Lp (a)), and shifts LDL particle size and number from small, dense pattern B (atherogenic) to large, buoyant pattern A (non-atherogenic) LDL.
The other non-lipid mediated atheroprotective benefits of niacin have established it as a viable, safe and effective therapeutic agent for reducing cardiovascular events. (5)
The early perceptions of a trend towards ischaemic stroke with niacin in the AIMHIGH study were unsupported by the evidence, and the absence of such a trend in a meta-analysis by P. Lavinge and R. Karas ( 6) confirms its use as an effective agent to reduce coronary heart disease risk.
NIACIN PLUS STATIN:
Combinations of niacin and a statin, likewise, have demonstrated improvements in a variety of surrogate endpoints, as in Arbiter 3 – (7) and Arbiter 6 – HALTS (8) .
The efficacy and safety of combination tablets of niacin extended release with simvastatin, compared to simvastatin alone, were demonstrated in the SEACOAST Study. (9)
Since the clinical efficacy and safety of Nicene has not been called into question in these and several other studies, the combination of niacin and a prostaglandin, raises questions about the potential off-target effects of laropiprant.
Notably, the FDA Adverse Event Reporting System has found prescription Nicene to be safer than simvastatin, pravastatin, atorvastatin, gemfibrozil and fenofibrate. (10), thereby confirming a significant clinical role for nicene in the treatment of mixed dyslipidaemias.
LAROPIPRANT EFFECTS ?
The safety of laropiprant in combination with a statin has never been demonstrated, raising questions about the potential adverse effects of laropiprant on atheroprotective pathways.
Laropripant blocks DP1 receptors on vascular cells and thereby prevents flushing, but it may also have unwanted effects on other DP1 receptors located on platelets and epithelial cells in the lungs and respiratory tissues.
STATIN EFFECTS ?
Statins too, have been shown, in some cases, to promote coronary artery calcification, a risk marker for cardiovascular disease.
Despite their observed benefits in some secondary prevention studies, ( unrelated to their LDL lowering potential,) their pleitropic effects may include other effects which are potentially detrimental, and which may explain the increased prevalence and extent of coronary artery calcification, by as much as 52%, in statin users compared to non-stain users. (11).
The widespread incidence of nerve and muscle damage in statin users has been extensively documented, and the mechanisms whereby such damage occurs has been proposed by Seneff et al. (12)
The significantly higher prevalence of coronary artery calcification in patients with type 2 diabetes is seen more frequently in statin users than in non-statin users (13), and the higher risk for new onset diabetes in statin users has been the subject of recent FDA warnings. (14)
The failure of Ezetimibe /Simvastatin, in the Enhance Study, (15) to reduce the atheroma burden in 720 patients with Familial Hypercholesterolaemia, despite a 58% reduction of LDL from baseline with the combination, and a 41% reduction in LDL with Simvastatin alone, raises questions about the potential for the combined therapy, or Ezetimibe alone, to advance, rather than impede, atherosclerosis in some patients.
EZETIMIBE EFFECTS ?
We don’t know what proportion of subjects in either group were given Ezetimibe in place of the combined statin therapy, and to what degree any potential off target effects of Ezetimibe might have influenced the outcome.
Ezetimibe has been shown by some researchers to trigger pro-atherogenic gene regulation mechanisms, including the inhibition of scavenger receptor B1 (SRB1) and ATP – binding cassette transporter A1 (ABCA1), giving rise to unintended consequences. (16)
Other studies, however, show no such effect on these genes. (17).
HDL BENEFITS:
While it is well established that HDL-C level is an inverse predictor of cardiovascular risk, it remains to be shown whether HDL per se, or specific sub-groups of HDL, or other factors associated with HDL elevations, are responsible for the observed reductions in cardiovascular events.
Increases in HDL LEVELS of 5%-26% were independently associated with a reduction in cardiovascular events in several trials. (16) (17) (18) (19) (20) (21) suggesting thereby a preventative role for strategies that augment HDL-C levels.
CONCLUSIONS:
The failure of TREDAPTIVE to show a statistically significant beneficial effect in HPS2-THRIVE may be due to several factors linked to the design of this study, with a soup of ingredients in the treatment arm, any one of which, in combination with the other, could have obscured any potential benefit in that arm.
The preliminary results of this trial are insufficient to dissuade clinicians from targeting low HDL as a risk factor for cardiovascular disease, or from using Niacin (nicotinamide) to augment HDL-C levels in at risk patients.
Dr. Neville Wilson, The Leinster Clinic, Maynooth, Ireland. (30 January, 2013).
REFERENCES:
- www.thrivestudy.org
- JACC Dec 19, 2012.
- Current Athero Rep 2000 (2) 36-46.
- Am J Cardiol 2007 (100) S53-S61.
- Am J Cardiol 2008 (101) 20B-26B.
- JACC March 27, 2012, vol 59, issue 13.
- Current Med Res Opin 2006 (22) 2243-2750.
- JACC 2010 (55) 2721-2726.
- J Chem Lipidol 2008 (2), 79-90 Pub Med.
10. Am J Cardiol 2008 (101) 9B-13 B (US FDA Adverse Event Reporting Database).
11. Atherosclerosis Aug 24, 2012 – VADT.
12. Seneff S. How Statins Really Work. (seneff@csail.mit.edu)
13. Diabetes Care 2012, 8 Aug.
14. FDA. Gov. FDA Expands Advice on Statins Risk.
15. NEJM April 3, 2008. Enhance Study.
16.J Nutr 2005; 135: 2305-2312.
17.J Atheroscler Threomb2007; 14: 99-108.
18. Circulation 1984:69 (2) 325-337. Coronary Intervention Study.
19.JAMA 1984:251 (3) 365-374. Lipid Research Clinics Program.
20.JAMA 1988:260 95) 641-652. Helsinki Heart Study.
21.NEJM 2001:345 (22) 1583-1592.
22.Circulation 1998;97 (15) 1453-1460. 4S Study.
23.JAMA 2001; 285 (12) 1585-1591.
ooooOOOoooo