by Dr. Neville Wilson
IODINE is an essential micronutrient. It is required by every cell in the human body, and although only small amounts are needed, by the cells of the various tissues, a deficiency in those cells will fail to protect them from potentially harmful and damaging toxins to which they are exposed.
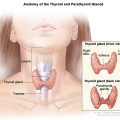
The human thyroid and breast are 2 of the body’s main storage sites for iodine, yet it is present in every cell, where it serves a structural and protective function. Iodine is a trace element which is present in variable amounts in the earth’s crust, and where iodine is sufficient in the soil, it may be found in a variety of common dietary items. Iodine, in its natural form, is scarce in many parts of the world, often leading to a variety of developmental disorders in children, such as cretinism, in which severe brain damage in early life can occur, or goiters and infertility in later years.
It has been estimated that one third of the world’s population lives in iodine deficient areas, and as much as 72% of the world’s population is affected by an iodine deficiency disorder. Iodine deficiency has been linked to thyroid and breast disorders, and medical records as far back as 1906 show that it was used in the past for a variety of medical conditions, including uterine fibroids, prostate hypertrophy, atherosclerosis, and even mercury, lead and arsenic poisoning.
Iodine it is essential for the synthesis of the thyroid hormones, in the thyroid gland, where it is extracted from the blood stream in its reduced form (iodide), and then oxidized to form iodine, which is then attachment to the amino acid L- Tyrosine, to form the various thyroid hormones, which are essential to life. 
The uptake of iodide from the circulating blood stream is performed by the outer wall of the thyroid cell, and transported into the inner wall of the thyroid cell, where the synthesis of the thyroid hormones takes place. Iodine is found in very small quantities in all the cells of the body, but it is only in the thyroid gland that it is used to synthesize the highly specialized thyroid hormones. The oxidation of iodide to form iodine is an important step in the process of synthesizing thyroid hormones, and requires the interaction of hydrogen peroxide (H2O2) and the enzyme thyroperoxidase (TPO).
H2O2 is a potent oxidizing agent, and in any other human cell it would cause damage to the cell. Within the thyroid gland, however, there is a unique chemical arrangement, whereby the cell is protected fro the generation of hydrogen peroxide. Since H2O2 is both essential for the formation of thyroid hormones, it is also potentially harmful to the cell, and its harmful effects need to be neutralized, a process which is effected by the selenium containing enzyme glutathione peroxidase.
Following the oxidation of iodide to iodine, Glutathione peroxidase reduces H2O2 to water (H2O) and oxygen (O2). The iodination of L-Tyrosine gives rise to 2 compounds, Monoiodothyronine (MIT) and Diodothyronine (DIT), which in turn become coupled to form the 2 active thyroid hormones, Triiodothyronine, or T3, and Tetraiodothyronine, or thyroxine, also designated T4. After the synthesis of these thyroid hormones has taken place, they are stored in the thyroglobulin inside the lumen of the cell follicle, shich then becomes a reservoir for the storage of the hormones, until they are required for use by the body.
The normal healthy thyroid gland stores about 8000 micrograms of iodine, 90% of which is in the form of MIT, DIT, T3 and T4. The remaining 10% is in the form of iodide. The release of these hormones occurs as thyroglobulin is broken down, and T3 and T4 released into the circulation, leaving T1 and T2 behind, which are then broken down to enable the release of iodide from tyrosine to take place.
Some of the iodide is released back into the circulation, while the remaining iodide remains within the cell to be recycled for the reformation of MIT and DIT. The normal thyroid will release about 80-90 micrograms of T4, and 6-8 micrograms of T3 on a daily basis. T4 acts as a prohormone, and is 300% less active that T3, which is the biologically active hormone, and which alone exerts its beneficial actions at receptor sites on all the peripheral cells of the body’s tissues.
SELENIUM :
Selenium is a trace element that is essential for health, and must be provided in the diet or in supplemental form, since it is not manufactured in the human body. Dietary levels of Selenium are dependent on selenium containing foods, which are in turn dependent on soil levels from which plants are obtained. Brazil nuts contain 544 ug per ounce of Selenium, while lower levels may be obtained from Tuna, Beef, Cod Turkey and whole wheat bread.

The RDA for selenium is 55ug per day for adults, but higher daily intakes are required to neutralize the toxic effects of H2O2 within the thyroid cell (thyrocytes), While H2O2 is essential for converting reduced iodine (iodide) to oxidized iodine, it may also cause cellular damage, and selenium containing glutathione peroxidase is the unique protective mechanism designed to safely reduce H2O2 to water and oxygen (H2O +O2) after it has oxidized iodide.
Selenium is also essential for the formation of 11 enzymes, two of the better known being glutathione peroxidase and iodothyronine deiodinase. Glutathione peroxidase reacts with Hydrogen peroxide to form water and oxygen, but requires adequate levels of selenium to perform this function. A selenium intake of 200 – 400 micrograms (ug) daily is required to protect the thyroid cells from oxidative damage, as well as from the toxic effects of common environmental agents, that may be ingested or inhaled, such as chlorine, bromine, fluoride, and pesticides, as well as mercury, arsenic and other heavy metals, of which any may pose a threat to normal thyroid function.
Selenium also plays an essential role in the action of certain enzymes required to activate and deactivate thyroid hormones. These belong to the family of DEIODINASES. The iodothyronine deiodinases (D1,D2 and D3) add, or remove, iodine atoms to the amino acid tyrosine, to form the various thyroid hormones, 3-mono-iodothyronine (T1), 3,5-di-iodothyronine (T2), 3,5,3’-tri-iodothyronine (T3), 3,5,3’,5’-tetra-iodothyronine (T4), and 3,3’5’-tri-iodothyronine (rT3 or reverse T3). The seleno-proteins require co-factors to be present for their actions, without which they may not be effective. These Co-factors are essential minerals, like magnesium, zinc, calcium, copper and chromium, and the B complex vitamins, and Vitamins A, C and E. High doses of Vitamin B2 (100 mg) and Vitamin 3 (500mg) and Vitamin C (3000 -10,000 mg) may be required in cases of insufficient hormone production and increasing symptoms of hypothyroidism.
IODINE DEFICIENCY:
When iodine levels are adequate in the thyroid gland it will contain approximately 15-20 mg, and concentrate its iodine through a highly specialized system called the sodium/iodide symporter, a mechanism also employed in breast tissue, and whereby iodide is transported into the cells (thyrocytes).
Iodine deficiency remains one of the major causes for hypothyroidism, with the depletion of natural iodine sources in some regions of the world, giving rise to thyroid goiters and thyroid hormone deficiency. In developing countries iodine deficiency is the leading cause of goiter and mental retardation. Iodine blocking pollutants have become another major factor in iodine insufficiency, with the insidious human exposure to environmental toxins, such as bromine, fluorine and chlorine, which being halogens, like iodine, block cellular receptive sites for iodine, causing insufficient uptake of iodine by the cells. Natural supplies of iodine from seaweed may also have been compromised by polluted seawater, caused by heavy metal and oil spillage, and contamination from the Fukushima Japanese nuclear reactor explosion in Chernobyl, in April 1986.
According to the WHO, iodine deficiency affects 72% of the world’s population. Up to 1960 the average slice of bread contained 150 micro-grams of iodine , in the form of potassium iodate. This level satisfied the RDA requirements of 150 mcg to prevent the occurrence of goiter, but not enough to provide optimal health protection. In 1970 iodine (in the form of iodate) was removed from flour, and replaced by bromine, which effectively blocked the effects of iodine, and may have been implicated in the escalation of female breast cancer, which in 1968 was 1:20, and in 2006, 1:7
IODINE MEDICINAL BENEFITS ?
The subject of iodine supplementation continues to be one of controversy, and may be linked to the Wolff-Chaikoff effect, which resulted from a false premise that iodine was a harmful product and to be avoided. The Wolff-Chaikoff Effect was described by 2 Californian Physicians, Drs Ian Wolff and Israel Lyon Chaikoff, as a temporary inhibition of thyroid hormone synthesis, supposedly occurring after increased thyroid ingestion. Some individuals, who have taken doses of iodine in excess of 50 mg per day, have reported mild swelling of the thyroid gland, but without any clinical symptoms of an under active thyroid gland.
In some cases the mild swelling has been accompanied by a mild elevation of TSH (Thyroid Stimulating Hormone) but without the effects of an underactive thyroid gland. Under these circumstances, TSH levels may remain elevated for a limited period and return to normal again. TSH is the hormone produced by the Pituitary gland which signals the thyroid to produce hormones (T4 and T3) when circulating levels are low. Elevated TSH levels usually indicate a state of thyroid under activity (hypothyroidism), while depressed TSH levels may indicate a state of over activity, or sufficient hormone production by the thyroid gland.
According to Dr. David Brownstein, MD. many patients are currently taking iodine supplementation, under the care of knowledgeable physicians, in dosages ranging from 10 to 200 mg per day, without any adverse symptoms, and with reported health benefit, and alleviation of previous symptoms and disability. The medicinal benefits of dietary iodine is supported by evidence from Ancient Chinese cure books, Egyptian Papyrus and antique medical preparations and pharmacy records. (The Iodine Crisis, p112- Lynne Farrow )
Archaeological findings in ancient societies, such as the Monte Verde village in Chile, have recovered evidence that prehistoric people consumed seaweeds for physiological and health protective effects. These findings have been replicated in ancient Chinese medicine practices which reveal the anti-viral and immune stimulating effects of iodine. More than a century ago American soldiers involved in the civil war conflicts carried iodine supplies to counter the septic effects of war wounds.

And today, countless reports of cures, for a multiplicity of medical disorders, are being reported by grateful patients, whose lives have been restored by iodine supplementation. Researcher Lynne Farrow has documented a large body of evidence, contained in testimonies from such patients, in a useful publication, called The Iodine Crisis. Medical researchers Guy Abraham MD, David Brownstein MD, and Jorge Flechas MD, are today leading the field in the resurrection of this ancient cure, which has largely, and unfortunately, escaped the attention of modern medical practitioners, depriving needy patients of a useful therapeutic option for a host of debilitating medical conditions.
Dr. Guy Abraham, is founder of the Iodine Project, which serves to inform and guide health professionals and patients, in the use of medicinal iodine for a wide range of medical disorders. Dr. Abraham states, “ The essential element iodine has been kept in the Dark Ages over the last 60 years after World War 11. We need to remedy the gross neglect of this essential element by the medical profession, poorly represented in medical textbooks and vilified in endocrine publications” ( Healing with Iodine, p3 – Dr. Mark Stone)
THYROID HORMONES AND IODINE :
The thyroid hormones are essential for energy production in every cell of the body’s tissues and organs, and are dependent on adequate iodine for their synthesis and metabolic effects. Elemental iodine can easily be reduced or oxidized. It is trapped in the thyroid circulation in the reduced form as iodide, and incorporated into the large complex protein, thyroglobulin, where it is oxidized to form iodine, and then, combined with the amino acid Tyrosine, as shown above, to form the thyroid hormones that control and maintain human cellular metabolism and function.
While iodine is concentrated in other tissues, such as the breast, uterus, ovaries, prostate, salivary glands, gut, cerebrospinal fluid, and parts of the eye, its highest concentration is within the thyroid gland. The presence of iodine in the thyroid circulation provides for protection of the thyroid against bacterial and viral infections. Triiodothyronine (T3) is the biologically active hormone that is carried through the circulation to every tissue cell for energy production.
The relatively inactive Tetraiodothyronine (T4) acts as a storage hormone, and will signal the hypothalamus and pituitary to release more thyrotropin releasing hormone (TRH) and thyroid stimulating hormone, (TSH) if circulating T3 is insufficient for cellular metabolic requirements. Inorganic iodide/iodine is non-radioactive, and tissue protective, and can be safely used in dosages of between 12.5 and 50 mg per day. Under supervision, as these dosages are significantly higher than the recommended daily allowance (RDA).
Thyroid hormones are essential for life, as they regulate key biochemical reactions, by increasing intra-cellular oxygen consumption, and regulating mitochondrial protein synthesis, as well as enzyme activities in target organs, such as the developing fetal brain, the thyroid gland, pituitary, heart, liver, kidney and muscles. Iodine protect against the effects of radio active Iodine : The Chernobyl accident in 1986, released many radio-active isotopes into the atmosphere and surrounding oceans, including the potentially harmful release of I-129 and 1-131 at the same time.
Although radioactive iodine 1-131 has a short half life of 8 days, compared to 1-129, which has a half life of 15.7 million years, both forms of radio active iodine pose a continuing threat to human safety and wellness. Many studies report an increase in thyroid cancer in children following the Chernobyl accident, due to the release of 1-131. But the release, also, of 1-129 into the environment means that large areas of water and food supply are likely to be contaminated for years to come. Since 1-131 and 1-129 travel together, both the short lived and the long living radioactive iodine have serious implications for generations to come. Radioactive iodine does not disappear.
It simply transmutes into other potentially forms. As 1-131 decays it transmutes into other radioactive elements such as radioactive Xenon gas , and Cesium, and then transmutes into a range of toxic heavy metals, which can be absorbed by human tissues, and concentrated in the thyroid gland and intracellular DNA of vulnerable human beings, causing genetic disturbances. (Geochemical Journal 2012;46:327-333) and organ malfunctions. Since inorganic, non-radioactive iodine protects and maintains the normal architecture of tissues in which it is present, it can protect against radiation damage to the body, while at the same time exerting an apoptotic effect by inhibiting the growth of cancer cells within the human body. In a paper by Dr. Bernard Eskin (Can J Surgery1993;36(5):453-460) iodine supplementation was shown to alter gene expression in breast cancer cells, inducing programmed cell death.
Several studies (Kunin, Zhang) show similar effects in lung and testicular cancer, as Iodine induces cancer cells apoptosis and remission. The rates of breast cancer and skin cancer have escalated over the past 30 years, and may reflect a dietary depletion of iodine, as well as iodine receptor blocking by the abundance of environmental halogens, like bromine, chlorine and fluoride, which are competitive inhibitors of cellular iodine receptors.
According to Prof Donald Muller, at the University of Washington, the ductal cells in the female breast, an area of likely cancer growth, are equipped with an iodine pump (Sodium-Iodine Symporter, similar to the one in the thyroid gland, which absorbs protective iodine. He says, “ today 1 in 7 American women will develop breast cancer during their lifetime. Thirty years ago, when Iodine consumption was twice as high as it is today, 1 in 20 women developed breast cancer”.
Several studies have shown that a low intake of iodine is associated with a high incidence of breast cancer, and a high intake of iodine is associated with a low incidence of breast cancer. Life expectancy among Japanese women, who consume seaweed as part of their regular diet, have a much lower rate of breast cancer than women who consume an iodine depleted western style diet.
Iodine deficiency allows the formation of precancerous nodules to develop, while iodine sufficiency can protect the breast, thyroid, uterus, ovary, and prostate architecture and also programme cancer cell death in these organs. Dr. David Brownstein, cites a large body of evidence to support his thesis that high dosages of iodine are safe, and effective as antibacterial, antifungal, antiviral agents, and afford protection against toxic environmental agents like bromide, chlorine and fluoride.
Because breast tissue concentrates iodine in the oxidized form, as iodine, and not in the reduced form, iodide, as concentrated by thyroid tissue, a combination of both forms is likely to benefit women who wish to use iodine as a protection against breast cyst formation and cancer.
Dr. David Brownstein recommends either Lugols or Iodoral as they both contain both forms of iodine. The use of combined iodine, according to Dr. Brownstein, also supports maintenance of the correct balance of estrogen in the female, thereby offering protection against an imbalance between estrone, estradiol and estriol, that may lead to mood swings and fibrocystic disease, and more serious disorders of the breasts, and the skeletal and cardiovascular systems.
A recent study reports that combined iodide/iodine therapy can favourably influence the gene expression in breast cancer, thereby lowering the risk of developing breast cancer. Since breast tissue is vulnerable to the effects of many environmental estrogens and xenoestrogens , iodine deficiency will increase the sensitivity of breast tissue to these toxic influences, and increase the risk for developing breast cancer. It makes good sense, therefore, to resort to the proven protective properties of iodine, in the form of combined iodide/iodine.
The prolonged threats to human health of radioactive iodine raises questions about the safety of conventional treatment for thyroid cancers, when employing radioactive iodine for diagnostic and therapeutic purposes. According to the Environmental Protection Agency, radioactive iodine can be absorbed through ingestion or inhalation, and can settle in several glands, including the thyroid. Since radioactive iodine is used in many medical diagnostic and treatment regimens, the potential risk of absorption and organ damage cannot be diminished.
According to the Journal of the American Medical Association. There are more than 40,000 new cases of thyroid cancer reported in the USA every year. And the number continues to escalate annually. Between 1990 and 2008, the percentage of patients treated with radioactive iodine climbed from 40 to 56%, and with the escalation of thyroid cancer incidence, questions must be asked about the possibility of over treatment of thyroid cancer by radioactive iodine.
MEDICAL TREATMENT WITH RADIOACTIVE IODINE:
According to a study outcome in Cancer, researchers are questioning the need to treat patients with early, low risk thyroid cancer with radioactive iodine, which does not increase their chances of survival, while putting them at risk for a secondary cancer.
According to Dr. Ian Ganly, a co-author in the study, “There is no need to expose these patients to any risk from radioactive iodine” Radioactive Iodine treatment for thyroid cancer continues to find favour amongst many Oncologists in Ireland and the UK, and the American Thyroid Association endorses it also, despite the risk of inducing cancer in the salivary gland and bone marrow by radioactive iodine treatment.
Patients undergoing CT scans may likewise be at risk, given that a single CT scan of the chest is equal to about 350 chest x-ray exposures. Hashimoto’s Thyroiditis and Iodine therapy: Hashimoto’s thyroiditis is an autoimmune disorder of the thyroid gland, resulting in a spectrum of debilitating, and often disabling, symptoms, caused by thyroid hormone deficiency, resulting from damaged thyroid tissue. Auto antibodies are mobilized by the immune system, in response to damaged TPO, which then attack healthy thyroid tissue, casing damage to the gland, and adversely affection hormone production.
The blood will reveal low levels of thyroid hormones (T4 and T3) and elevated levels of thyroperoxidase antibodies (TPO ab) Under attack by antibodies, surrounding thyroid proteins may also be damaged, including the protein thyroglobulin, resulting in raised blood levels of Thyroglobulin antibodies (TG ab) and depressed hormone production, resulting in clinical hypothyroidism. As shown above, TPO is required for the conversion of iodide into iodine, and if TPO is damaged, the process will be impaired and iodine will not be formed, and thyroid hormones not formed.
Under conditions of hypothyroidism caused by iodine deficiency, supplementation with iodine or natural dessicated thyroid hormone (NDT) has beneficial outcomes. Natural dessicated thyroid hormone products, such as Naturethroid, NP Throid, Westhroid and Armour, have been used widely, and successfully, to supplement the deficient supply of thyroid hormone from a damaged thyroid gland. Hashimoto’s thyroiditis is a form of hypothyroidism, caused, not by iodine deficiency, but by auto-immune antibodies, which attack and destroy thyroid tissue.
Controversy surrounds the question of whether supplemental iodine should be given to patients who have autoimmune Hashimoto’s thyroiditis. While iodine supplementation is not routinely prescribed by conventional doctors, patients who have taken personal responsibility for their thyroid care may be confused by statements from some authors who recommend iodine restriction for people with Hashimoto’s thyroiditis.
Concerns about iodine supplementation in cases of Hashimoto’s thyroiditis are based on the view that when TPO is damaged by TPO antibodies, additional iodine intake will provoke more TPO synthesis, and in turn, attract more antibodies, thereby perpetuating the damage to the thyroid gland inflicted by the auto-antibodies. Researcher and author Isabella Wentz (Hashimoto’s Thyroiditis) supports this view, citing experimental mouse models who spontaneously (without iodine) developed TPO antibodies, and when given iodine in water, developed increased levels of thyroiditis.
We are not told, however, whether other influences, such as goitrogens, or toxins, were present in their diet. She also cites a Korean study, in which 78 out of 90 hypothyroid patients regained normal thyroid function after restricting their iodine intake to less than 100 mcg per day. She also concedes that flaws in this study did not make for a compelling argument, as selenium levels were not assessed during the study, and the presence of halogens, like fluorine and bromine was not evaluated, and no account was taken of the fact that many of the Korean subjects may have included iodine-rich foods in their diet.
We know that halogens have the tendency to occupy iodine-binding sites, affecting the absorption, distribution, metabolism and excretion of iodine, and producing symptoms of iodine deprivation, such as hypothyroidism. Datis Kharrazian, author of “Why Do I Still Have Thyroid Symptoms ?” does not recommend Iodine for Hashimoto’s patients, basing his argument on the fact that because iodine stimulates the production of TPO, more TPO will attract more antibodies, and the Hashimoto’s condition will worsen.
He states that adding iodine under these circumstances is “like throwing gasoline onto a fire”. (NEJM 1995;333(25):1688) and that some people may develop symptoms of an overactive thyroid (NEJM 2000;343(17):1236), while others will have no symptoms despite tests showing an elevation of TPO antibodies. Kharrazian cites studies which show an increase in the rate of Hashimoto’s in countries such as China, Turkey and Sri Lanka, when iodine supplementation is used to correct iodine deficiency in those countries.
He does however acknowledge that when large doses of iodine are taken the production of TPO will be shut down. This means less TPO to attract an autoimmune response. However, shutting down TPO production will inhibit thyroid hormone production, and may reduce symptoms of an overactive thyroid, as in hyperthyroidism. Dr. David Brownstein (Iodine, Why You Need It) is a proponent of megadoses of iodine, to treat hypothyroidism, and also to reduce the risk of certain cancers. He does, in so doing, state that certain provisions are required.
- Ingest enough iodine in order to provide adequate substrate to iodinate lipids.
This may require 6-50 mg per day, and exceeds the RDA for iodine of 150 micrograms per day.
2. Take vitamins B2 and B3 in amounts necessary to stimulate the NADPH system to produce adequate amounts of H2O2.
This may require Vitamin B2 (100 mg) and Vitamin B3 (500 mg) twice a day to stimulate ATP production and provide adequate H2O2 for the oxidation of iodide.
3. Correct oxidant stress in the thyroid gland and the mitochondria with antioxidants.
This may require high dosed Vitamin C (3000-10,000mg per day).
4. Ensure adequate magnesium levels.
5. Minimize oxidative stress in the body.
This may require drinking adequate amounts of pure water and eating a healthy diet every day (Iodine-Why You Need It-David Brownstein, – pp173-176)
IODINE AND CANCER PROTECTION:
Because iodine can function as an oxidant and anti-oxidant , it can function effectively as an anti-cancer agent and offer protection against cancer in the human breast and thyroid gland. (Biofactors,19.2003) (Cell Biochem Funct , 18.2000)
IODINE also has the ability to induce death of cancer cells, known as apoptosis, in both breast and thyroid cells. (Endocrin141,2000) Since iodine can be incorporated into cellular lipids, to form iodo-lipids, it may help to stabilize cellular membranes and afford them protection against toxic alteration. The metabolism of Iodine (reduced iodine) can follow 2 pathways.
- It can be oxidized to form iodine, and be used to manufacture the thyroid hormones.
- It can undergo organification, whereby it is bound to an organic molecule, such as a lipid or a protein.
Organification does not occur at low intakes of iodine, such as at the RDA level of 150 mcg/day, but with higher dosages of iodine . The RDA level of 150 mcg/ day is the lowest nutritional requirement to prevent goiter formation. Higher doses than the RDA may be required to maintain optimal thyroid function and protection of Thyroid, Breast, Uterine and Prostate against
In a recent 2000 study, researchers show that the iodination of lipids of the cell membrane requires the oxidized form of iodine, rather than iodide, and that iodine may play an important role in the protection of the cell and mitochondrial membranes against free radical damage, by iodination of unsaturated lipids in the membranes. (Prog Nutr 2000;2;15-19, Cocchi M et al)
Dr. Neville Wilson.
September 2018


Excellent summary which I think surpasses Dr. brownstein’s book which I found basic and repetitive although it woke me up to the importance of iodine for other cells than thyroid. Thanks for doing so much work on this and have I your permission to share with patients? Joan. (Medical Herbalist and Nutritional Therapist)
Thank you so much for this article, it is most useful. I am suffering from hypothyroid for many years and often felt very poor. My quality of life is low because of this condition. It is getting better now, when I found information online about iodine deficiency. And because doctors like you share this information. It would be great to know your opinion on what standard tests patients with hypothyroid should undertake to monitor their condition. Many thanks.
Thank you Olivia. I am pleased to note that your health has improved.
It would be prudent to have your Urine Iodine output checked to ensure that you have adequate iodine stores for your thyroid to function optimally.
You can have the test done through the Biolab Medical Unit at email:info@biolab.co.uk
You need to have a urinary iodine excretion of between 100 and 199 micrograms per litre.
Other important tests are: Free T3, Free T4, TSH, TPO antibodies and Tg antibodies, as well as Vit D3 and Vit B12, plus Iron studies.
Hopes this helps !
Dr Nev.