Dr. Neville Wilson. 4th September 2020
In a recent Pilot Study, conducted in Spain, Vitamin D supplementation reduced the risk of being admitted to Intensive Care Unit (ICU) in a way not previously reported, and also eliminated the risk of death from Covid-19 infection. (1)
While the health benefits of Vitamin D have been long established, this is the first randomized controlled trial of Vitamin D to be published with special reference to patients infected with Covid-19 (SARS-Cov-2).
In the Spanish Study 76 patients with Covid-19 viral pneumonia were randomized into 2 groups, with 50 patients receiving Vit D orally, and 26 patients not being given Vit D supplementation.
Dosages of 25-hydroxyvitamin D3 were given in dosages of 0,532 mg caps daily for the first week, and then 0,266 mg daily on day 3 and day 7, and daily thereafter.
In addition, all patients were given antibiotics, in accordance with current standards of care, as follows : Hydroxychloroquine 400 mg 12 hourly for 1 day, then 200 mg 12 hourly for 5 days, plus Azithromycin 500 mg daily for 5 days, and Ceftriaxone 2 g iv every 24 hours for 5 days.
The group being given Vit D3 (Calcifediol) recorded a significant risk reduction for ICU admission, and a likely reduction of risk for death from COVID-19 infection.
There were some differences in participants in the 2 groups compared, with more participants in the control group having high blood pressure and diabetes, and more people in the vitamin D group being over age 60 years, with 5 times more having had previous organ transplants.
Adjusting for these differences, vitamin D reduced the odds of admission to ICU by 97% with the 95% confidence interval ranging from a 75%-99.7% reduction in the odds.
All the vitamin D patients were discharged without complications.
Half of the control group was discharged without ICU admission, while the remaining half 11, who were admitted to ICU, were eventually discharged and 2 died later.
The group who supplemented with vitamin D had a reduced risk of being admitted to the intensive care unit (ICU) and a reduced risk of death following infection with COVID-19
While Vitamin D3 (Cholecalciferol) is the nutritional substrate for Calcifediol, the latter was used in this pilot study because of its superior intestinal absorption, and can rapidly restore serum concentrations of 25-hydroxy- D3, (25(OH)D3) since it does not need to be hydrolyzed in the liver as occurs with 25(OH)D.
The current method of determining Vitamin D status is a blood measurement of 25(OH) D which is not the active form, but an inactive metabolite of the active form that was used in this clinical study.
The Different Forms of Vitamin D :
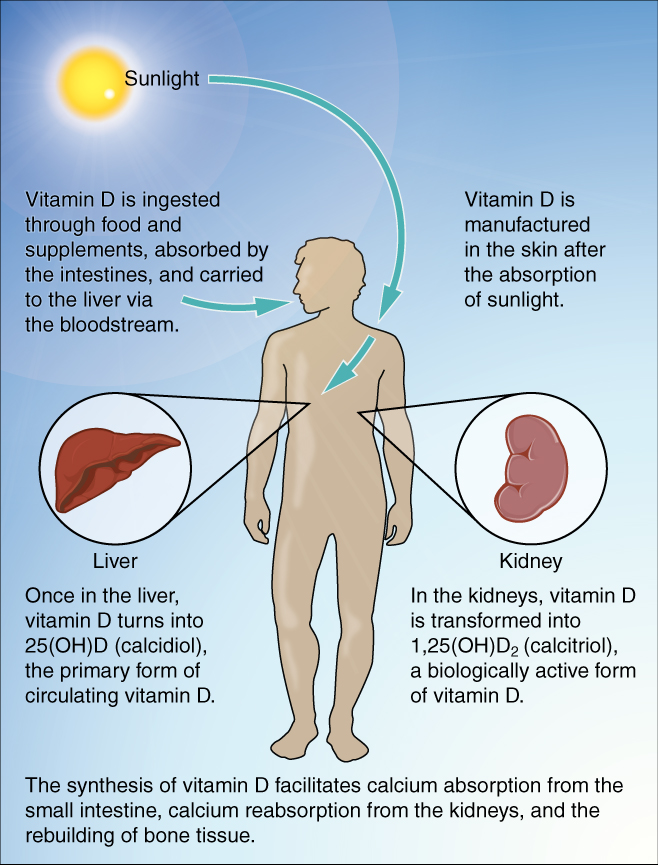
Vitamin D is not actually a ”vitamin”, but a prehormone, and in its natural and supplemental form, is turned into 2 very important hormones, called calcidiol and calcitriol, which are chemically different, and have different functions in the human body.
The naturally occurring vitamin D, when sunlight stimulates the bare skin is called cholecalciferol, and large quantities are made in the skin when exposed to ultraviolet (UVB) rays from the sun, prompting the conversion of cholesterol (7-dehydrocholesterol) in the deep layers of the skin to cholecalciferol (vitamin D3).

This biochemical transformation of cholesterol into life supporting hormones illustrates clearly the vital role that cholesterol plays in human biological protective mechanisms.
Cholecalciferol (vitamin D3) :
This is the original form of vitamin D3, and from which the other forms, are generated , as metabolites, each with specific metabolic functions.
In addition to natural occurring cholecalciferol, we can also ingest cholecalciferol from animal sources (D3) or vegetable sources, in the form of ergocalciferol (vitamin D2).
In either form it is a fat soluble nutrient, primarily absorbed in the small intestine, by passive diffusion, and then delivered, via enterocytes, into the lymphatic system, and then into the circulation, where it is attached to vitamin D binding proteins, (DBP) for further transport to target tissues and organs. At this stage cholecalciferol is still inactive.
In order for it to be active, it must be extracted by the liver cells, where it is converted into calcidiol (25-hydrocholecalciferol), a prehormone, by enzyme hydroxylation with CYP2RI (25-hydroxylase) and is not yet an active hormone.
Calcidiol ( 25(OH)2D3 or 25D3)
This inactive prehormone is the most prevalent circulating form of vitamin D, in the blood, and is therefore the form in which vitamin D3 is measured, following extraction of a blood sample.
Vitamin D blood levels, as reported by doctors, refers to this form of vitamin D. However, it needs to be further metabolized into its active form, in the kidney, where it is converted, by hydroxylation, (renal 1-alpha-hydroxylase) to Calcitriol, the active form in which it is utilized by the body for a wide range of biochemical processes that regulate various human physiological functions.
Calcidiol is bound to vitamin D binding protein (DBP) in the circulation and has a half life of 15 days, compared to the active form, Calcitriol, which is measured in hours and not days.
Calcitriol (1,25(OH)2D3 or 1,25D3)
Calcitriol (1,25-dihydroxyvitamin D) is the biologically activated form of vitamin D, and is the most potent steroid hormone in the human body, having a wide range of protective and physiologically supportive functions for human health enhancement.
The physiological benefits of vitamin D, as listed below, are due to Calcitriol activity, even though blood levels are measurements of circulating Calcidiol.
SUPPLEMENTAL Vitamin D3 and D2 :
Vitamin D supplements may be available in the form of vitamin D3 (cholecalciferol) or vitamin D2 (ergocalciferol), the latter being the form in which some non-prescription supplements have been widely available in the past.
Ergocalciferol (D2) is derived by radiating fungus and is not the naturally occurring vitamin D for humans, and is often found in some multivitamin preparations.
There is some evidence that ergocalciferol is more toxic in overdose than cholecalciferol, since it is more rapidly metabolized than cholecalciferol, and this may account for the concerns about vitamin D overdosage, which in the form of cholecalciferol is unlikely.
It is important for consumers to realize that ergocalciferol is a drug and does not occur naturally in the human body.
Dose Requirements :
Current studies indicate that for adults 4000 units (100 micrograms) of cholecalciferol a day is required to meet the body’s requirement for vitamin D, but protective and therapeutic dosages will depend on individual blood levels and physiological requirements.
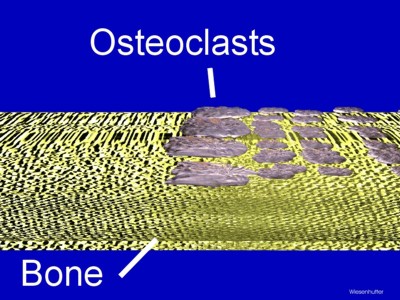
Historically, attention has been focused on the role of vitamin D in bone metabolism, where 1,25(0H)2D can stimulate osteoblasts, increase calcium ion absorption from the kidney tubule, and gut, and stimulate the formation of new cancellous bone.
The discovery of vitamin D receptors (VDR) in a wide variety of human cells stimulated an interest in the role of 1,25(OH)2D in immune function and host defence in many common disorders, including heart disease, diabetes and cancer.
The protective role of vitamin D in several common health disorders is considered hereunder.
Vitamin D Deficiency and Disease:
The protective and therapeutic benefits of vitamin D for human health has led to an increasing awareness of widespread insufficiency in and across population groups, given the lack of exposure to adequate sunshine in many communities globally, and also the increased risk of disease, resulting from inadequate dietary provision or supplemental use by many vulnerable people.

The risk for vitamin D insufficiency is increased in these cases, as well as where human metabolism is less efficient due to increased demand, as in old age, pregnancy, or several common medical conditions.
Risk Factors for Vitamin D Deficiency :
- The inappropriate incident angle of the sun, affected by latitude, season and time of day.
- Persons with dark skin, or those using excessive sunscreen protection. (2)
- Persons using prescription medication that can deplete vitamin D levels, such as metformin for diabetes, proton pump inhibitors for reflux oesophagitis, steroids and anti-convulsant drugs.
- Modern diets lacking in healthy fats, required for the absorption of fat soluble vitamin D.
- Persons with digestive impairments or malabsorption disorders, (IBD) and those who have had a small bowel resection.
- Obese persons since vitamin D is fat soluble, and fat deposits may lead to less bio-available vitamin D in the circulation.
- Pregnancy and Breast – feeding females.
- Babies and young children under the age of 5 years.
- The elderly with lower levels of skin 7-Dehydrocholesterol.
What is the Optimal blood level of Vitamin D ?
In a small cross sectional observational study in the Philipines, vitamin D levels below 29 – 34 ng/ml (72.5 – 85 nMol/L) were found to be associated with more severe COVID-19 outcomes.
In this first observational study of vitamin D effects on COVID-19 infection 90% of severe and critical outcomes occurred at 25(OH)D levels under 30 ng/ml (75nMol/L) whereas 97.5% of mild cases had 25(OH)D above 30 ng/ml (75nMol/L).
Mild cases were defined as having no pneumonia, where severe cases were defined as having respiratory distress, and critical cases as having respiratory failure and requiring admission to ICU.
This study was a preprint reported on 09 April, 2020, by researcher Mark Alipit.
Vitamin D3 levels are determined by measuring the 25 (OH) D form , and this can be achieved by obtaining a venous sample, or capillary droplet test from a finger prick, for which specialized kits are available.
Different categories of level are used to determine optimal levels and deficiency levels, as well as sufficient levels or insufficient levels.
The following are a guide, but personal requirements may determine target levels.
Optimal levels: In excess of 50 ng/ml of blood (125 nmol/L)
Sufficient levels : At least 30 ng/ml of blood. (75 nmol/L)
Insufficient levels : Blood levels of 21-29 ng/ml (52.5 – 72.5 nmol/L)
Deficiency level : At or below 20ng/ml (50 nmol/L)
EVALUATING DAILY INTAKE AND POTENTIAL TOXICITY FOR VITAMIN D :
An evaluation of vitamin D intake up to 15000 IU/ day and serum levels of 25(OH)D up to 300 nMol/L was conducted by researchers investigating potential for toxicity and harm, and concluded that these targets were appropriate for health and without evidence of toxicity. (3)
Because of toxicity concerns the Institute of Medicine (IOM) set a target of 4000 IU as the tolerable upper level of daily intake. (4)
Early studies have shown that as much as a daily intake of 5000 IU vitamin D3 may be required to achieve a serum level of 100 nMol/L (5)
The safety of serum levels of 25(OH)D as high as 500 nMol/L have previously been reported, with no evidence of toxicity. (6)
An ideal target for normal physiology was proposed by Heany as being 100-130 nMol/L for 25(OH)d intake. (7)
Masai herdsmen, who spend most of their day in sunshine, have levels in the range of 100-150 nMol/L, a level that may be achieved with an oral intake of 5000 IU to 10,000 IU daily.
While the IOM has set a safe target for daily intake at 4000 IU , the USA Endocrine Society Practice Guidelines recommend up to 10,000 IU daily for adults. (8)
In 2011 the Endocrine Society agreed that levels of 25(OH)D up to 250 nMol per day was not associated with toxicity, and that vitamin D3 toxicity is likely only at serum levels in excess of 375 nMol/L. (9)
TESTING FOR VITAMIN D SUFFICIENCY:
An estimated 1 billion people worldwide do not have adequate Vitamin D levels, and populations in countries situated north of 37 degrees latitude are particularly compromised by having limited exposure to the natural solar provision of ultraviolet (UV-B) radiation required for the synthesis of vitamin D in the human body.
Unfortunately, people who live in sunny parts of the globe, may also be at risk of vitamin D insufficiency , by spending prolonged periods of daylight hours indoors, by wearing protective clothing when outdoors, or excessive “lathering” of sunblock when outdoors, or by inadequate intake of dietary selections containing Vitamin D, such as oily fish, full-fat milk and eggs.
Modern diets are unlikely to provide adequate amounts of Vitamin D3 because of the trend to eat “low fat “ foods, as has been recommended by many doctors in recent years, and also the large scale avoidance of vitamin –D- rich foods like naturally reared poultry, organic eggs, and fatty fish such as kippers, herrings and salmon.
Sun avoidance combined with current dietary practices are likely causes for the widespread escalation of vitamin D deficiencies.
A recent study revealed that even in sunny Australia 58% of Australians suffer from vitamin D deficiency (10) and similar trends have been uncovered in some European countries such as Portugal, Hungary and Italy.
Surprisingly, 65 % of the Portuguese population have low levels of vitamin D and 15% have severe deficiency, while Hungarian population studies reveal an insufficiency rate of 60%, and in Italy, a popular holiday destination for sun seekers, 60%-70% of children and adolescents are moderately to severely deficient of vitamin D. (11)
Unfortunately, the common practice of lathering sun exposed areas of the human body with potent sun screen applications, as recommended by many healthcare professionals, may unwittingly, block the beneficial absorption of vitamin D by the skin.
The unfortunate avoidance of dietary fats by so many people, following decades of misguided public dietary guidelines would have compromised their natural absorption of Vitamin D, since Vitamin D is fat-soluble and requires adequate dietary fat intake for its optimal absorption.
These groups of people, with insufficient levels of circulating Vitamin D would benefit greatly by supplementing regularly with an appropriate strength of quality grade Vitamin D3 nutrient.
Dark skinned people, too, are likely to produce lower levels of circulating Vitamin D, and would also benefit from supplemental Vitamin D intake.
Obesity, a common global phenomenon, or a body mass index (BMI) in excess of 30, is likely to increase the level of stored Vitamin D in body adiposity, resulting in lower blood and tissue levels of vitamin D.
Gastro-intestinal disorders, such as Irritable Bowel Disease (IBD), or liver disorders, may likewise, decrease the absorption of vitamin D from the gut.
Inadequate supplemental Vitamin D resulting from inferior quality, or inadequate daily dosage, may likewise lead to insufficient circulating levels of vitamin D, thereby increasing the risk for a wide range of debilitating medical disorders, such as heart disease, respiratory ailments, diabetes, Alzheimer’s Disease, Parkinson’s Disease, and some forms of cancer.
Unfortunately Vitamin D deficiency is a global epidemic, and remains a critical risk factor for poor health in many unsuspecting persons, whose vitamin D status is not regularly checked or addressed with appropriate supplementation.
Tragically, Vitamin D assessment has not been routinely conducted in Ireland, with Government labs often rejecting physician requests for Vitamin D tests on grounds of budgetary restriction.
Establishing patient levels of Vitamin D is still not standard of care in many clinical settings, leaving large numbers of patients in the dark regarding their vitamin D status and immune potential.
Clinical studies show that vitamin D deficiency is associated with increased risk for a long list of common diseases that span all systems in the body.
It has become evident that high doses of vitamin D are required to interact efficiently with vitamin D receptors (VDR) throughout the human body, and thereby support vital functions in heart muscle, brain cells and bone matrix.
While vitamin D has long been regarded as the “bone vitamin”, early studies by Drs Wacker and Holick have identified the positive effects of supplementation for skeletal and extra – skeletal health. (12)
DIETARY SOURCES OF VITAMIN D :
While the richest source of Vitamin D is ultraviolet – B radiation (UV-B) from sunlight, certain foods can serve as dietary sources, the richest among which is cod liver oil, providing 5.7 milligrams of cholesterol per gram of food.
Other dietary sources of vitamin D are chicken liver, egg yolk, butter and fatty fish, like sardines, shrimp, mackerel and oysters.
For food sources to provide optimal levels of vitamin D they need to be sunlight exposed, with UV-B radiation.
Because vitamin D, like vitamin A, K and E, is fat soluble it is more efficiently absorbed in conjunction with a fatty meal.
Vitamin D can also be synthesized from plant sterols and occurs in a form called “ergocalciferol”, or Vitamin D2, which may be the form used in some “Vitamin D” supplements, but does not provide the health benefits offered by cholecalciferol (Vitamin D3) which is the true Vitamin D formed by sunlight exposure by humans and animals.
TRANSPORT OF VITAMIN D :
Following the synthesis of natural Vitamin D from sunlight exposure, or absorption from vitamin D-rich fatty animal foods, and supplemental D3, it needs to be bound to a protein carrier for distribution throughout the body.
Vitamin D-binding protein (DBP) acts as a transport carrier for the hormonally active 1,25 hydroxyvitamin D, and also serves as a reservoir and buffer of 25(OH)D to prevent too rapid delivery of the steroid to the target cells, thereby preventing toxicity, and controlling availability in accordance with the body’s requirements.
For this reason toxicity from high doses of Vitamin D3 is rare, and more likely to occur with vitamin D2, (ergocalciferol) which has a lower affinity for the vitamin D-binding protein (DBP) and is not as well bound and preserved as is vitamin D3 (cholecalciferol) .
The weaker affinity of vitamin D2 metabolites to DBP produces higher and more biologically available proportions of free 25(OH)D2 and 1,25-(OH)D2, and may thus be responsible for the greater risk of D2 toxicity as a result. (13)
Although vitamin D2 has been the form used in many pharmacological preparations in the past, significant differences in metabolic activity between vitamin D3 and vitamin D2 clearly demonstrates that they are not equivalent on a per mole basis, and not interchangeable, leading to the conclusion that vitamin D2 should no longer be regarded as a nutrient appropriate for supplementation or fortification of foods.
The inefficiency of vitamin D2, compared with vitamin D2, at increasing 25(OH) D is now well documented (14)
In a 2006 study the use of vitamin D3 showed a small but statistically significant benefit in improving all-cause mortality among elderly women, compared to use with vitamin D2. (15)
Vitamin D2 (ergocalciferol) was not shown to confer a mortality benefit in a 2014 Cochrane meta-analysis despite adequate statistical power. (16)
Vitamin D and Bone Health:
It is widely accepted that a biological function of vitamin D is to increase calcium and phosphorus absorption, and thereby support bone health metabolism.
It has long been established that adequate vitamin D intake protects and preserves bone health in females and males, when taken with other supporting nutrients like calcium, magnesium, vitamin K2, and zinc.
These nutrients, in combination, help to protect against Osteopenia and Osteoporosis, by building strong bones and reducing the risk for bone fractures in the elderly.
Bone health in infants and adolescents is of equal importance, given the recent findings of an 18 year old study by Danish researchers, that more than half of newborn babies have insufficient levels of Vitamin D required for normal growth and development of their skeletal system.
The widely held view that Vitamin D is only linked to bone health is shortsighted and misguided, since Vitamin D is vital for many important physical functions in the human body.
Vitamin D and Nervous System :
Calcium levels are vital for a normal functioning nervous system, and serum levels are kept within a narrow optimum range by the parathyroid glands, which indirectly affect vitamin D (Calcitriol).
Parathyroid hormone (PTH) secreted by the parathyroid glands monitors serum calcium and controls the level of the l- hydroxylase enzyme in the kidney, which determines the synthesis of Calcitriol in the kidney.
Calcitriol in turn normalizes serum calcium and enables the intestinal absorption of dietary calcium to be optimized, increasing absorption from 10%-15% to 30%-40%.
Calcitriol, the active form of vitamin D, works with PTH to stabilize serum calcium, by increasing re-absorption, and supporting nervous system efficiency. (17)
Vitamin D and Heart Health :
A 2010 study revealed that vitamin D insufficiency is widespread in individuals with cardiovascular disease. (18)
An earlier 2009 study revealed the benefit of vitamin D in “inducing an antifibrotic phenotype in mesenchymal multipotent cells” thereby reducing the risk for strokes and sudden death. (19)
The MONICA/KORA Study in 2013 revealed that low levels of serum 25-hydroxyvitamin D are associated with increased risk of myocardial infarction (heart attack) and that women with higher levels enjoyed a 68% lower risk, while males with higher levels enjoyed a 44% lower risk. (20)
The wide distribution of vitamin D receptors (VDR) in heart muscle, blood vessels and respiratory tissues, indicates the need for adequate levels in these tissues for optimal function and protection against disease. (21)
VDR cells are present in vascular endothelium, vascular smooth muscle and cardiomyocytes and may protect against atherosclerosis through inhibition of cholesterol uptake and foam cell formation, reduced vascular smooth muscle cell proliferation, and reduced expression of adhesion molecules. (22)
Hypertension (high blood pressure), a risk factor for cardiovascular disease, and COVID-19 INFECTION, is inversely associated with vitamin D levels. (23)
Lowering elevated Blood Pressure was achieved by raising 25(OH)D either by supplementation or UVB exposure. (24)
A 2009 study identified the beneficial role of vitamin D in reducing risk markers for cardiovascular disease, with a 13.5% reduction in serum triglyceride by supplementing with 3,320 IU of vitamin D3. (25)
The dosage level of vitamin D intake is important for ensuring cardiovascular protection and continuing heart health.
Studies of cardiovascular patients who take 400 to 600 IU vitamin D reveal no benefit, whereas taking 2000 IU or higher daily provided the desired protection. (26)
In a 2002 Australian Study at least 2000 IU daily was required to ensure the minimum target of 30 ng/ml of vitamin D in subjects being investigated. (27)
The protective role of vitamin D3 for vascular health was demonstrated in a 2011 study on the role of vitamin D in peripheral arterial disease. (28)
Vitamin D lowers the Risk of Diabetes:
Diabetes has been identified as a significant co-morbidity in people who have been infected with the Coronavirus SARS 2 (Covid-19), and studies reveal that people with Type 1 and Type 11 Diabetes have lower levels of vitamin D than the general population. (29)
It is not unlikely that the widespread distribution of Diabetes as a comorbidity in those infected with COVID-19 may have been vulnerable because of low Vitamin D intake and low Vitamin D levels.
In a 2013 Epidemiological Study vitamin D deficiency was shown to double the risk of progression to full blown type 11 diabetes. (30)
These early studies reveal that vitamin D deficiency has long been known to be implicated in a range of physical disorders that are clearly associated with compromised immunity and vulnerability to Covid-19 infection.
The distribution of vitamin D receptors (VDR) in the Beta cells of the pancreas , (which produce insulin) as well as in the liver, fat and muscle tissue enable vitamin D sufficiency to maintain their optimal function of regulating insulin and glucose balance. (31)
Vitamin D sufficiency for Insulin synthesis was demonstrated in early rat studies with D3 deficiency causing reduction in de novo insulin biosynthesis. (32)
Even macrophages, the white blood cells that are part of the human immune system, have vitamin D receptors (VDR) which enable vitamin D uptake as a protective measure against excess fat accumulation by macrophages.
Laboratory treatment with vitamin D of macrophages taken from diabetic patients demonstrate a reduced uptake of fat indicating a reduction in risk for cardiovascular disease. (33)
This is another example of how vitamin D sufficiency protects macrophages from excess fat accumulation and reduces the risk of cardiovascular disease.
VITAMIN D supports IMMUNITY :
Vitamin D status enhances innate immunity and inhibits the development of autoimmunity. (34)
In a 2013 paper researchers report that vitamin D regulates chemokine production, counteracting autoimmune inflammation, and inducing differentiation of immune cells to promote “self tolerance”. (35)
In a systematic review of randomized controlled trials in 2009, researchers reported the protective benefits of vitamin D against various infections, especially tuberculosis, influenza and viral upper respiratory infections. (36)
These findings were replicated in a 2012 study showing that vitamin D enhances the innate immune response against various infections. (37)
In a 2013 Pilot Study the benefits of vitamin D were observed in the induction of monocyte differentiation, and inhibition of lymphocyte proliferation, as well as the production of cytokines, including interleukin 1 and 2.
Vitamin D also suppressed immunoglobulin secretion by B lymphocytes, and enhanced the activity of some vitamin D-receptor positive immune cells and the sensitivity of certain target cells to various cytokines. (38)
A randomized controlled trial in 2010 showed that school children taking supplemental vitamin D (1200 IU daily) significantly reduced their risk of seasonal viral influenza. (39)
In a 2015 study researchers observed that vitamin D plays a role in the normal immune response and in modifying immune mediated diseases. They focused on the molecular mechanisms involved and concluded that vitamin D is a key factor in regulating both innate and adaptive immunity. (40)
Vitamin D exerts profound effects beyond its classical functions on bone metabolism, with many studies confirming the capacity for vitamin D to down-regulate pathological immune responses in patients who have autoimmune or inflammatory disease.
A systematic review published on 24 September 2019 describes the role of vitamin D in increasing circulating T regulatory cell numbers and modulating T regulatory cell phenotypes in patients with inflammatory disease or in healthy volunteers. (41)
In an Israeli population based study, including 14,000 members, low plasma levels of 25(OH)D defined as below 30ng/ml, were associated with increased risk for COVID-19 infection. (42)
In a recent study (2020) Boston University researchers reviewed CRP levels (serum markers for inflammation), and vitamin D levels in hospitalized patients with COVID-19 infection, and found that only 9.7% of patients older than 40 years who were vitamin D sufficient, succumbed to COVID-19 infection, compared to 20% who had circulating levels of 25(OH) D less than 30 mg/ml. (43)
These findings, correlated to CRP levels, suggest that vitamin D sufficiency may help to modulate the immune response by reducing risk for cytokine storm in response to COVID-19 infection.
In this study patients who were vitamin D sufficient had significantly lower levels of CRP and a higher total blood lymphocyte count, suggesting that vitamin D sufficiency had improved their immune function and protection against COVID-19 infection.
A Wide Range of Health Benefits offered by Vitamin D :
Drawing on decades of research into the health benefits of Vitamin D, Dr. Michael Hollick, PhD., M.D. stated, more than a decade ago, “ Today there is evidence to link sun exposure and vitamin D to every facet of medicine and health. Adequate levels of vitamin D can improve fertility, safeguard pregnancy, reduce inflammation, help with weight control, protect against infections, diseases like flu and tuberculosis, prevent strokes and dementia, bolster the immune system, boost memory, and support muscle strength”. (44)
Added to these observations are outcomes from recent studies showing the protective benefits of vitamin D for several common human cancers, including the following :
- Breast Cancer : (45) (46) (47) (48) (49) (50)
- Prostate Cancer : (51) (52)
- Colorectal Cancer: (53) (54)
Cancer cells have lower VDR s than other cells, leaving them incapable of regulating inflammation, and therefore less likely to undergo apoptosis (cell death). (55)
Autism-Spectrum Disorder (ASD) and vitamin D deficiency:
An increased risk for Autism-spectrum disorder (ASD) in children born of mothers deficient in vitamin D during pregnancy was revealed in the 2018 Generation R Study in Netherlands. Researchers established a link between vitamin D deficiency during pregnancy and autism in their offspring children. (56)
CONCLUSION :
Vitamin D enjoys a range of protective benefits in human physiology, as well as therapeutic benefits in common chronic medical conditions.
There is compelling evidence that vitamin D has a vital role to play in health management, and under the present conditions of global corona virus (COVID-19) transmission and increased risk for respiratory infections in susceptible persons, the inclusion of vitamin D in risk reduction strategies should be a priority.
Administration of calcifediol or 25 hydroxyvitamin D to hospitalized patients with COVID-19 infection significantly reduced their need for Intensive Care (ICU) admission, by reducing the severity of their disease. (1)
Dr. Neville Wilson, MB ChB, D Obs, D Fam Med, MSc.
4 September, 2020.
REFERENCES :
1. The Journal of Steroid Biochemistry and Molecular Biology – 29 Aug 2020,105751, Castillo ME et al
2. www.drnevillewilson.com- Prescriptions for Summer.
3. Dermato – Endocrinology 2017, vol 9, No1, Kimball SM et al.
4. J Clinical Endocrinol Metabolism 2011; 96 (7): 1911-30, Holick MF.
5. Nutrients 2015;1(12): 10189-208, Veugelers, PS, et al.
6. Am J Clin Nutr 2007, 85;6-18, Hathrock J, et al.
7. J Endocrinol Invest 2014 2014; 37 (11):1127-30, Heany RP, et al.
8. J Gen Intern Med 2002; 17(9): 733-5, Holick MF, et al.
9. J Chem Endocrinol Metab 2011;96 (7): 1911-30, Holick M et al.
10. The Australia Health Survey (AHS) 2011-2013
11. Nutrients 2018; May; 10(5): 546
12. Nutrients 2013 Jan 10:5 (1): 111-148, Wacker M, Holick MF.
13. Am J Clin Nutr 2001; 73:288-94, Vietch R et al.
14. Am J Clin Endocrinol Metab 2004;89: 5387-91 Armas LA, et al.
15. Am J Clin Nutr 2006 Oct 84 (4): 694-7, Houghton LA, et al.
16. Cochrane Data Base Syn Review 2014, Jan 10;1 CD007470, Bjelakovig G etal.
17. Archives of Biochemistry & Biophysics 523 (1),73-76, Christakos.
18. Mol Nutr Food Res 2010, Aug: 54 (8), 1103-13, Pilz S et al.
19. J Endocrinol 2009 Feb 200 (2): 207-21, Artazal N, et al.
20. J Clin Endocrinol Metab 2013 Jan;98 (1): 272-80, Karakas M, et al.
21. Clin Endocrinol (Oxf). 2011 Nov; 75 (5): 575-84 Pilz S et al.
22. Heart 98 (8), 609-614, Reid R et al.
23. J of Hypertension 29, 2011,(4) 636-645, Burgaz A.
24. Lancet 1998, 352 (9129), 709-710 Kraine R.
25. Am J Clin Nutr 2009 May; 89 (5): 1321-7, Zitternan A, et al.
26. J Clin Endocrinol Metab 2010, Oct ; 95 (10) 4584-9, Dong V.
27. J Clin Endocrinol Metab 2012 Dec 97 (12): 4473-80, Tran B et al.
28. Vasc Health Risk Manag 2011, 7 :671-5, Chu GT et al.
29. Endocrinol Metab Clin North America 2010 June; 39 (2): 419-46, Takishi J et al.
30. Cardiovasc Diabetol 2013, 12:17, Huang Y.
31. Endocrin Metab Clin North Am 2010, June 39, (2): 419-46, Takishi J.
32. J Endocrinol 1999; 160:87-95, Bourion PM et al.
33. Arculition 2009, Aug 25; 120 (8): 687-78.
34. Annual Review of Nutrition 2003, 117-145, Griffin MD et al.
35. Nutrients 2013,5 (1), 111-148, Wacker H.
36. Endocrine Practice 2009, 153 (5), 438-449, Yamshchikov A.
37. Vit D and the Lung. NY Human Press PD 59-84
38. J of Translational Medicine 2013, 11: (176), 1-7 Ojami S.
39. Am J of Clinical Nutrition 2010, 91 (5), 1255-1260, Urishima M.
40. Nutrients 2015 Sept 24; 7 (10): 8251-60, RanWe.
41. Plos One Sept 24, 2019, Fisher SA et aL.
42. Med RXiv 3 July 2020, Merzow E et al.
43. Plos One Sept 25, 2020.
44. The Vitamin D Solution by Michael F. Holick. P xxii
45. J Natl Cancer Inst. 2012, Dec 19: 104 (24); 1897-904, Amaral AF et al.
46. Breast Ca Res Traet 2013 Jan; 137 (2): 559-607, Bilinski K, et al.
47. J Steroid Biochem Mol Biol Aug 23, Krishna AV.
48. Steroids 2012 Sept; 77 (11):1107-12, Krishnan AV.
49. Am J Clin Nutr 2011 Oct; 94 (4):144-9, Bollard MJ.
50. Nutr Cancer 2011; 63(6):827-41, Brunner RL et al.
51. J Clin Endocrinol Metab 2012 July; 97(7): 2315-24, Marshall DT, et al.
52. Endocrinol 2012 June; 153(6): 2576-87, Swami S et al.
53. Cancer Res Prev (2011) Oct; 4(10):1645-54, Hopkins MH, et al.
54. Cancer Re Prev (2012) Oct; 5 (10): 1247-56, Ahearn TU et al.
55. Best Pract Res Clinic Endoc Metab 2011, Aug:25(4):593-604, Els v.
56. J Molecular Psychology. 23,240-246 (2008), Vinichuyzen AA et al.
00000
Dr. Neville S. Wilson.
4th September, 2020